Most people assume that antibiotics kill bacteria, but leave human (and other eukaryotic) cells unscathed. Unfortunately, this assumption isn’t correct. Bactericidal antibiotics have been found to damage the mitochondria of human cells.
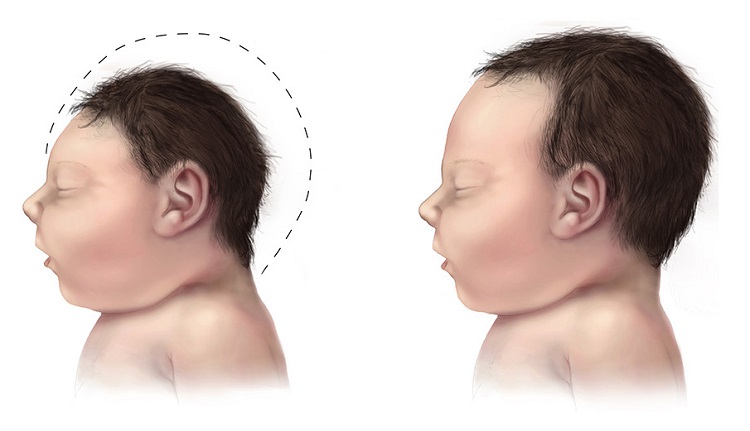
Mitochondria are present in almost every cell in the body (except for red blood cells and sperm). They are responsible for cellular energy production, cell signaling, apoptosis (the process through which the body kills unhealthy cells), and aging. Mitochondria are vitally important organelles and malfunctioning mitochondria have been linked to many diseases including fibromyalgia, chronic fatigue syndrome / M.E., autism, Gulf War Syndrome, Alzheimer’s Disease, Parkinson’s, diabetes, cancer, and others.
Focusing on Fluoroquinolones
Though several kinds of bactericidal antibiotics have been shown to damage mitochondria, I’m going to focus this article on fluoroquinolone antibiotics because, a) there are multiple journal articles that note that fluoroquinolone antibiotics damage mitochondria, b) fluoroquinolone antibiotics have been shown to not just damage mitochondria, but to deplete mitochondrial DNA as well, and c) adverse reactions to fluoroquinolones involve multi-symptom, chronic illness that typifies mitochondrial injury.
Fluoroquinolone antibiotics – cipro/ciprofloxacin, levaquin/levofloxacin, avelox/moxifloxacin and floxin/ofloxacin – are damaging human mitochondria. This has been shown repeatedly, and even the FDA (never first to the party) acknowledges that the mechanism for damage done by fluoroquinolones is mitochondrial damage and the ensuing oxidative stress that occurs when mitochondria are damaged.
FDA Report Notes that Fluoroquinolones Damage Mitochondria
In their April 27, 2013 Pharmacovigilance Review, “Disabling Peripheral Neuropathy Associated with Systemic Fluoroquinolone Exposure,” the FDA notes that the mechanism for action through which fluoroquinolones induce peripheral neuropathy is mitochondrial toxicity. The report says:
Ciprofloxacin has been found to affect mammalian topoisomerase II, especially in mitochondria. In vitro studies in drug-treated mammalian cells found that nalidixic acid and ciprofloxacin cause a loss of motichondrial DNA (mtDNA), resulting in a decrease of mitochondrial respiration and an arrest in cell growth. Further analysis found protein-linked double-stranded DNA breaks in the mtDNA from ciprofloxacin-treated cells, suggesting that ciprofloxacin was targeting topoisomerase II activity in the mitochondria.
The FDA Pharmacovigilance Report also notes that mitochondrial damage (and the ensuing oxidative stress that occurs when mitochondria are damaged) is related to multi-symptom, chronic diseases like optic neuropathy, neuropathic pain, hearing loss, muscle weakness, cardiomyopathy, lactic acidosis, Parkinson’s, Alzheimer’s and amyotrophic lateral sclerosis (ALS).
Bactericidal Antibiotics Damage Mitochondria
A study entitled “Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells” that was published in Science Translational Medicine in 2013 notes that:
Clinically relevant doses of bactericidal antibiotics – quinolones (fluoroquinolones), aminoglycosides, and Beta-lactams – cause mitochondrial dysfunction and ROS overproduction in mammalian cells. We demonstrated that these bactericidal antibiotic-induced effects lead to oxidative damage to DNA, proteins and membrane lipids. Mice treated with bactericidal antibiotics exhibited elevated oxidative stress markers in the blood, oxidative tissue damage, and up-regulated expression of key genes involved in antioxidant defense mechanisms, which points to the potential physiological relevance of these antibiotic effects.
Fluoroquinolones Deplete Antioxidants
Fluoroquinolone antibiotics damage the cellular mechanisms that are needed to repair mitochondrial damage – namely intracellular antioxidant production. The FDA report notes that, “Under normal circumstances, there is a mechanism to remove or prevent the generation of ROS to avoid cellular damage such as lipid peroxidation, mtDNA mutations, and DNA strand breaks; if this does not happen, it can then lead to even more oxidative damage.”
A 2011 study of Indian patients who took various fluoroquinolones to treat urinary tract infections found that, “There was substantial depletion in both SOD and glutathione levels particularly with ciprofloxacin.” SODs are superoxide dismutases – enzymes that are necessary for converting superoxide – a powerful oxidant – into oxygen and hydrogen peroxide. Without adequate SOD, superoxide wreaks havoc on every cell in the body. Glutathione is often called the “master antioxidant” and without proper levels of it, oxidants damage cells. (Additionally, “Glutathione (GSH) has a crucial role in cellular signaling and antioxidant defenses either by reacting directly with reactive oxygen or nitrogen species or by acting as an essential cofactor for GSH S-transferases and glutathione peroxidases. GSH acting in concert with its dependent enzymes, known as the glutathione system, is responsible for the detoxification of reactive oxygen and nitrogen species (ROS/RNS) and electrophiles produced by xenobiotics. Adequate levels of GSH are essential for the optimal functioning of the immune system in general and T cell activation and differentiation in particular.” source)
As the FDA noted, when damaged mitochondria produce too much ROS, and the mechanisms to limit the damage (cellular production of antioxidants) aren’t working properly, an increasing amount of oxidative damage is done. This is often referred to as the “vicious cycle” of mitochondrial damage – damaged mitochondria produce excess ROS (reactive oxygen species – often called oxidative stress), those ROS further damage the mitochondria, the further damaged mitochondria produce more ROS, and so on, and so on. As noted above, mitochondrial damage, oxidative stress, and the vicious cycle between them has been linked to every chronic disease that plagues people – diabetes, Alzheimer’s, autism, etc.
Fluoroquinolone antibiotics damage mitochondria and cause an increase in ROS/oxidative stress. They also deplete cells of antioxidants such as SOD and glutathione, leaving the cells unable to neutralize ROS / oxidative stress. Excess cellular ROS / oxidative stress is related to every chronic disease there is.
See Evil, Hear Evil, but do Nothing About It
Rather than utilizing the FDA’s vast databases and the hundreds of Ph.D. scientists and statisticians on their payroll to determine whether or not fluoroquinolones – which have been shown to cause mitochondrial damage and oxidative stress, are related to the many chronic diseases that plague Americans – diseases that have been shown to be caused by mitochondrial damage and oxidative stress; the FDA simply added one more thing to the 43 PAGE warning label for fluoroquinolones – PERMANENT PERIPHERAL NEUROPATHY. They could have, and probably should have, added warnings that noted that fluoroquinolone use increases the risk of every disease that is linked to mitochondrial damage and oxidative stress – Alzheimer’s, Parkinson’s, ALS, diabetes, autism, depression, etc.
But they didn’t. They just added another warning that few physicians will read let alone understand and left these drugs on the market.
Fluoroquinolone antibiotics – cipro/ciprofloxacin, levaquin/levofloxacin, avelox/moxifloxacin and floxin/ofloxacin – are damaging human mitochondria and inducing large amounts of oxidative stress that wreaks havoc on many areas of health. The FDA knows about this, and they are doing nothing about it. Actually, worse than doing nothing, they are increasing the length of the warning label, so that when victims go to sue the companies (Bayer makes Cipro and Avelox and Johnson & Johnson makes Levaquin) that damaged their cells and gave them a multi-symptom, chronic disease, they are told that their symptoms are on the warning label and thus they gave informed consent to be crippled by an antibiotic.
It is absurd. Fluoroquinolones do severe damage to human cells, and the FDA is looking the other way. They’re not protecting our mitochondria, and they’re not protecting us.
Sources:
- Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology, Pharmacovigilance Review, April 17, 2013, “Disabling Peripheral Neuropathy Associated with Systemic Fluoroquinolone Exposure”
- Science Translational Medicine, “Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells”
- Journal of Young Pharmacists, “Oxidative Stress Induced by Fluoroquinolones on Treatment for Complicated Urinary Tract Infections in Indian Patients”
- Molecular Pharmacology, “Delayed Cytotocicity and Cleavage of Mitochondrial DNA in Ciprofloxacin Treated Mammalian Cells”
- Molecular Neurobiology, “The Glutathione System: A New Drug Target in Neuroimmune Disorders”
Information about Fluoroquinolone Toxicity
Information about the author, and adverse reactions to fluoroquinolone antibiotics (Cipro/ciprofloxacin, Levaquin/levofloxacin, Avelox/moxifloxacin and Floxin/ofloxacin) can be found on Lisa Bloomquist’s site, www.floxiehope.com.
Write for Us
Patient stories are important. Help spread awareness. Write for us.
Participate in Research
Hormones MatterTM is conducting research on the side effects and adverse events associated with the fluoroquinolone antibiotics, Cipro, Levaquin, Avelox and others: The Fluoroquinolone Antibiotics Side Effects Study. The study is anonymous, takes 20-30 minutes to complete and is open to anyone who has used a fluoroquinolone antibiotic. Please complete the study and help us understand the scope of fluoroquinolone reactions.
Hormones MatterTM conducts other crowdsourced surveys on medication reactions. To take one of our other surveys, click here.
To sign up for our newsletter and receive weekly updates on the latest research news, click here.
What Else Can I Do To Help?
Hormones MatterTM is completely unfunded at this juncture and we rely entirely on crowdsourcing and volunteers to conduct the research and produce quality health education materials for the public. If you’d like help us improve healthcare with better data, get involved. Become an advocate, spread the word about our site, our research and our mission. Suggest a study. Share a study. Join our team. Write for us. Partner with us. Help us grow. For more information contact us at: info@hormonesmatter.com.
To support Hormones Matter and our research projects – Crowdfund Us – Buy an Unsubscription.