When we salt our food, we rarely think of salt as a crucial aspect of our physiology. In particular, we think it has absolutely nothing to do with anything other than taste and we certainly do not think of hormones. In this short post, I would like to clarify a few myths about salt and salt types and hint at their importance and hormonal connection.
The Myths of Designer Salts
Myth #1 sea salt versus table salt. There are hundreds of posts on the Internet about the benefits of sea salt over table salt. I would like everyone to know that there is only one salt on planet earth: sea salt. The fact that it may be called table salt simply suggests that some time ago it was clearly understood by all that all salt came from the sea. There was no need to place the word “sea” in front of salt; we all knew what it was. Somehow we have forgotten that salt comes from the sea. Now many designer salts have showed up with the word “sea” in front of the word salt and sell for much more than table salt. Don’t be fooled: all salts come from the sea! Preferences, of course, may mean you pick a designer salt over table salt, but I would like to make sure you know that in terms of salt, they are the same for the body.
You may ask: how can they be the same for the body if one contains all kinds of other elements as well as pure salt itself. The answer is very simple. In the body, salt molecules (NaCl) break down into ions (Na+ and Cl-) and only these two ions participate in what is called voltage activated sodium pumps (Nav1.1-1.9) where 1.1 to 1.9 indicates that there are 9 such pumps and Nav stands for voltage activated sodium pump. Thus, for the body only ions matter. Na+ is inside the cell and is positively charged. Cl- is outside the cell and is negatively charged. The two create the voltage necessary for the cell to function. Some of these pumps also have additional functions—such as sending pain message when a pump opens and does not close properly. The influx of Na+ and Cl- can cause the signal of pain to go off causing chronic pain. Much is yet to be understood by the function of salt but the one thing we already know: salt is NaCl and no additional organic matter matters.
Myth #2 refers to rock salt that comes from mountains like the Himalayas in various colors. They make beautiful lamps but in reality they are sea salts that have fossilized as the tectonic plates have shifted and lifted the Himalayans out from under the sea. Why are they pink or orange and very colorful in general? Because as the mountains were lifted, pressure increased on the salt deposits and the weight of the mountain pressing heat and metals through the salt created fossilized salt with various metals trapped in the salt itself. There is nothing wrong with eating fossilized rock salt except that by the nature of the fossilization process of high heat, pressure, and the many metals, a large percentage of these “minerals” entrapped in the salt are actually radioactive metals. Again, it is a taste question whether you prefer Himalayan or other salt but know what you are getting.
Myth #3 is Celtic and similar sea salts of various colors that are collected from clay pools and evaporated such that each sea salt crystal has little cavities of entrapped water with “minerals.” I see many lists of minerals for various sea salts but few of us actually consider where those minerals come from. I know we all love to eat sea food, fish, shellfish, and sea weeds as well. The mineral deposits in designer sea salts come from the debris of these sea animals, including their excrement and dead bodies. There is nothing wrong with eating fish poo and dead fish as long as you know that your choice of salt contains it. Some of these salts are proud to also include a bit of clay, and hence, the moisture must be kept else you will need a hammer and chisel to break the salt up. So, much of the charm about designer salts is trickery and harmless misinformation that takes advantage of those who are not aware.
The truth: salt, by chemical composition Sodium-Chloride (Na+, Cl-) is only these two elements combined, as discussed above. Our bodies use these chemicals only in ionic form. Salt is part of the baby’s amniotic fluid in our bodies (not Himalayan salt, and not various colored sea salts; just simple Na+ Cl-). This standard chemical element constitutes a very large part of the over 70% saline brine of our bodies. We are made of salt water. When we visit the emergency room with any illness, the most often used first step – the needle with a clear liquid dripped into our vein – is also saline water electrolyte. Electrolytes contain other elements to complete the full list of micro and macro nutrients of the 70% brine.
Other Minerals in Salt
What about the so called “minerals” that are in the designer salts? Do we need them?
- Magnesium is a very important element that provides a key such that the cells can open at all given the proper electrical environment. Magnesium also provides crucial nutrient for the mitochondria (little bacteria in every single cell of our body that converts the food we eat to energy packets our cells can use). You get more magnesium out of a bite of food (just about any food) than from an entire box of designer salt.
- Calcium is needed for high voltage channels where the neurotransmitters are released.
- Potassium is needed to keep the balance of hydration in the cell and outside of the cell to ensure that the cell is not overly hydrated (potassium is a diuretic).
- Phosphates. We also need phosphates and other elements and of course a ton of water, but the elements in designer salt sold as essential mineral are minuscule and meaningless.
- Iodine. Another important factor is iodine. Designer salts do not contain iodine. In the US, the government has gone through great trouble placing iodine into our salt to eradicate goiter, a disease of the thyroid. Without adequate iodine our thyroid is not able to produce the right amount of hormone to keep our brain healthy. Recall also, in Japan after the nuclear plant released all that radiation, the first item sold out throughout the country was iodine. Iodine acts like a sponge, soaking up many toxins from our body to be able to eliminate them. Radioactivity is one of those things iodine can help clear from our bodies.
Salt and Hormones
So the question then is: what does salt have to do with our hormones? Does it matter? Indeed, it does. Those who have read the migraine series 3-part posts know that the most critical element in preventing and treating migraines is salt. Every single neuron in our brain has several voltage-gated sodium pumps (sodium-potassium pumps) to generate voltage. Without such voltage the neurons are not able to manufacture and release their neurotransmitters-hormones in the body. Thus, restricting salt in your diet retards the hormone manufacturing of your body. In previous articles, I showed how studies show that low salt diets are harmful even for those with preexisting heart conditions and hypertension. Salt does not increase blood pressure, provided that salt is consumed with sufficient amount of water, along with potassium and the other minerals and nutrients, I listed above.
Sodium retains water thereby hydrating the cells. Sodium chloride maintains the polarity differences between the inside and the outside of the cell membrane to control the electrical activity, which then open the pumps. Having enough salt in your brain makes the difference between having a headache/migraine or not. What if it also helps prevent other diseases of the brain? There are suggestions that fibromyalgia and neuropathy may be connected to one of the Nav pumps. I wonder if other conditions such as bipolar disorder, anxiety disorder, and even depression could be, at least partly, caused by an inappropriate level of sodium in the brain?
Possible Role for Sodium – Potassium Pumps in Disease
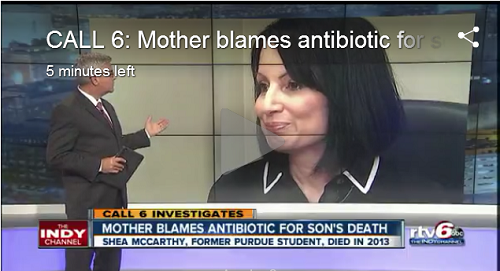
Let’s investigate one of the voltage activated sodium pumps. The one we seem to know most about so far: Nav1.7. According to recent research, this particular pump has a critical role in chronic pain dampening. Experiments on various poisonous animals—including the Chinese red-headed centipede and the snake black mamba—show that their venom seems to selectively choose this particular pump to dampen the pain associated with some types of chronic pain. The pain signals need not be located in any one particular location of the body, but are relayed by the brain as hormones release for the pain message. People with neuropathy, such as Type 2 Diabetes or those who have been been floxed (suffered an adverse reaction to a fluoroquinolone antibiotics) are very familiar with this pain. Nothing seems to help with this type of pain except a very few types of strong drugs of the brain, some (like Gabapentin) inhibit nearly all activities in the body in near-full-force. The drugs of the brain are systemic whereas the venom is capable of acting on only one sodium-potassium pump, the Nav1.7. Perhaps, in the future, this finding can be applied to reduce neuropathic pain without global nervous system dampening.
My Two Cents
I suspect most ailments of the central nervous system that include a hyper-sensitivity for pain will become a subject of sodium pump malfunction research. There are also indications that there is a switch in the connection of the peripheral nervous system to the spine, and thereby the central nervous system, where there should be a relay station to either inhibit or amplify the pain. Apparently, at this relay station the switch is flipped backwards and what should be inhibiting actually amplifies. Pain experienced from these crossed wires is called allodyna. I suspect we will be hearing much about this term in the future and how it connects to various sodium pump malfunctions that today we do not yet understand.
Sources:
Pain Scientific American December 2014; p:62-67