The New York Times reported that women are less satisfied with their health care than men, citing a study from Health Services Research.
Researchers could see an overall difference between men’s and women’s views, but these differences were even more prominent for particular questions. One question asked patients if they felt they received sufficient information for the medications they were prescribed, and the other question asked whether patients were satisfied with the cleanliness of the hospital.
In both cases, women were less satisfied with health care than men – significantly so. Now the question is, Why?
Perhaps women have just been paying attention to the news. Dr. Mark Hyman explains in the Huffington Post that postmenopausal women are being prescribed cholesterol-lowering medication that increases their chances of getting diabetes – by 71%.
This isn’t the only instance in which women’s health needs were overlooked:
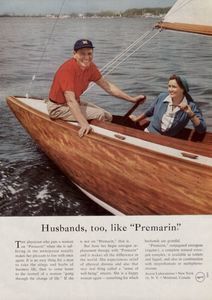
- Premarin was prescribed to postmenopausal women to prevent heart disease, but it increased their chances of having a heart attack.
- Studies have found increased osteoporosis in postmenopausal women prescribed osteoporosis medication.
- Women are prescribed medicine as though they’re men, yet they are more likely than men to have irregular heartbeats due to prescription cocktails.
- Many doctors don’t realize that pain medication does not have the same impact on women as it does on men. Experiments show Ibuprofen did not reduce pain for women.
- In fact, the Society for Women’s Health Research and Medco Health Solutions, Inc. presented a study that showed women are prescribed more medication than men, yet they are less likely than men to get the appropriate drug for their needs.
- The Center for the Study of Sex Differences at Georgetown University in Washington, D.C. explains that your gender can significantly impact how your disease should be diagnosed and treated. Yet the FDA only required that women be included in drug research since 1993.
No wonder women are less satisfied with their health care than men.
Women Are Less Satisfied with Health Care Provider’s Cleanliness
As it turns out, women’s immune systems are more resilient than men’s. Even so, women are more susceptible to certain illnesses and diseases than men are. Some experts suggest a woman’s stronger immune system is the cause for her susceptibility to autoimmune disorders, but the reasons remain unclear.
Sharyn Clough, a philosopher of science at Oregon State University, explained on NPR how society’s emphasis on a girl’s cleanliness could impact her susceptibility to diseases when she gets older, since she may not be exposed to the same bacteria as young boys.
While this may, or may not, be the case, it makes sense for a woman to be more aware of the cleanliness of her environment if she was raised to do so. It is even more reasonable for a woman to consider the cleanliness of her surroundings if she is more susceptible to disease – especially when she is in an institution that treats the sick.
It’s important that health care providers know that women are less satisfied with their health care than men. Voicing our opinions raises awareness, and these industries don’t want to lose half of their market.
It’s entirely possible that women are less satisfied with health care than men because women pay more for health insurance than men – health care that seems to be specifically geared toward the needs of men, not women.
Related Posts:
Women Pay More for Health Insurance
Affordable Care What’s in Effect Now
Falling Through the Cracks
This post was published previously in April 2012.