What is the anatomy of a migraine? Do migraines have an anatomy, a location map, in the same way heart disease does? Sure, migraine happens in the brain and we feel the pain in our head if there is pain – not all migraines come with pain, but does the pain guide us to a causative anatomy of the migraine the same way a heart attack does to the heart? No, it does not; at least not in the same way a blocked artery points to the cause of heart attack. The symptoms of migraines correspond to no specific regions of the brain, except in the case of the aura migraine, which points at the visual cortex. Only about 15% of those with migraines have auras. For 85% of the cases, we do not have the anatomical location of the migraine understood. Most science seems to consider aura and non-aura migraine different in nature and cause. Are they? Maybe not.
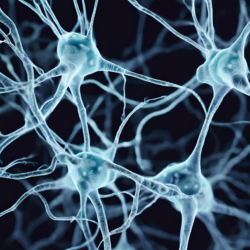
Most migraines are not connected to the symptoms we feel (nausea, dizziness, IBS, RLS, anxiety, nausea, vomit, etc.) and because of the variety of symptoms, there is nothing to guide us, such as a scan of the arteries for heart or a stroke. Another contributing factor is that there are no pain sensing nerves in the brain. All pain is felt by the trigeminal neuron receptors that are located on the meninges of the brain. That is, the pain we feel as migraineurs is disconnected from the actual location that causes migraines. To find the anatomy of a migraine, we need to go beyond the symptoms and the pain of the disease, beyond the visible disturbance of the eye in the aura, to the underlying cause for these symptoms.
For much of recent history, migraine research has revolved around two discrete theories of migraines: vascular and non-vascular mental illness. The two schools of thought were merged into what is now called neurovascular disease. But the latest findings suggest that there is more to migraines than neurovascular disease.
Migraine as Vascular Disease
For much of the 20th century, migraine was considered to be a vascular disease. This meant that migraine pain was caused by cranial blood vessel dilation or constriction. Still today we can see many over-the-counter migraine drugs that constrict blood vessels with caffeine in order to constrict the vascular structure of the brain (and the heart and the rest of our body). Alternatively, many doctors still prescribe beta blockers that reduce blood pressure and loosen arteries for easier blood flow and reduced constriction. If migraine is a disease of vascular nature, what causes the cranial vasodilation changes, particularly if these changes do not affect the heart or other parts of the body? This is the first clue that migraines are something more than just vascular in nature.
Migraine as Non-Vascular Mental Illness
The second prominent theory in migraine research attributes migraine pain to alterations in neurotransmitters, specifically, serotonin. Research is confusing on whether migraineurs have less or more serotonin than non-migraineurs. The possible serotonin connection brought us the many prescription drugs containing, increasing, or decreasing serotonin in the brain (triptans, SSRIs and others). Today, most migraineurs receive at least one serotonin enhancing drug; some I know receive serotonin blocking drug but that represents the minority. I was one of the millions of migraine patients who received serotonin enhancers (triptan) and also one of the millions of migraineurs for whom these medications did not work.
Again, I must ask, if there is a serotonin deficiency or overflow in migraineurs, what causes it? And if it is a deficiency as is proposed to be the case for most migraineurs, isn’t this the same proposed deficiency as in depression? Why then don’t most who are depressed also suffer from migraines or why do those who suffer migraines as a result of lack of serotonin not suffer depression? It is not clear to me that there is any connection between serotonin and migraine since most migraineurs I know are not at all depressed and most depressed do not have migraines. This tells me that something is not right with the concept of identical treatments for such two completely different illnesses.
Serotonin is created by a normally functioning brain. Why it is deficient, or in some cases, elevated in the brain of migraineurs has always puzzled me. It still puzzles me that others didn’t ask why neurons cannot produce the right amount of serotonin on their own or why physicians so easily prescribed drugs to add or enhance what the brain was not making. Should we not find out why the neurons are not producing serotonin in the first place? Wouldn’t this help us better treat and maybe even cure migraines?
Migraine and New Research
The most recent theory about migraines involves the aberrant electrical discharges associated with migraine and a phenomenon called cortical spreading depression:
Cortical spreading depression (CSD) and depolarization waves are associated with dramatic failure of brain ion homeostasis, efflux of excitatory amino acids from nerve cells, increased energy metabolism and changes in cerebral blood flow (CBF). There is strong clinical and experimental evidence to suggest that CSD is involved in the mechanism of migraine, stroke, subarachnoid hemorrhage and traumatic brain injury. (Lauritzen et al., J Cereb Blood Flow Metab)
Researchers have linked CSD to the eminent onset of migraine pain. Such a rapid change in brain ion homeostasis can affect changes in neurotransmitter concentrations, causing cranial vascular dilation and ionic imbalance with depolarized regions. These changes can evoke what migraineurs sense as pain but one has to ask by what mechanisms are these ionic brain changes initiated and by what pathways do they elicit the pain. For the first question, let us return to the concept of neural dehydration and salt deficiencies as possible instigators.
A Unified Theory of Migraine Pain
A new report shows migraines, seizures and strokes are all about ion (sodium, potassium, chloride, magnesium, and oxygen) homeostasis. These particular models looked at how changing potassium ion concentration affects brain activity and how seizures and migraines have similar underlying mechanisms. Potassium’s job is to work both inside and outside of the neurons helping to balance homeostasis by ensuring that potassium ions are in the correct place all the time. Potassium is a diuretic substance and helps in the removal of excess or used water from the cell. If there are too many potassium ions inside or outside of a neuron, with all else remaining constant, the neuron will end up dehydrated because of the osmotic gradient.
The overabundance of potassium and a depletion of both extra-cellular sodium chloride reduces water, and changes the pH balance (acidic level) of the neuron (Costa et al., The Journal of Headache and Pain). Recall from my earlier post: Dehydration and Salt Deficiency Trigger Migraines, that channels on the membrane of the neuron allow for leaks using osmotic gradient to balance the internal and external ionic content. Because ionic homeostasis balance is required for a healthy brain, the ionic balance must be true for all electrolyte elements, including sodium as well. Not enough sodium can cause a potassium overabundance that can trigger migraines because the neuron is not able to generate electricity or retain water.
In Dehydration and Salt Deficiency Trigger Migraines, I talked about the importance of hydration and explained how that works at the cellular level. I introduced the sodium-potassium pumps and their role in keeping the cell hydrated. Through the sodium-potassium pumps sodium ions and potassium ions head in and out of the neuron when proper electric currents are established. For the electric current, the ionic balance of sodium and chloride is essential so that the pumps can open and close. There are also osmotic channels through which leakage of ions may happen depending on higher or lower levels of ions inside versus outside the cell—the osmotic gradient.
The phenomenon of cortical spreading depression is a slow spreading electrical surge corresponding to depolarized regions of migraine initiating locations. It is initiated by ion imbalance where the normal homeostasis has been lost. Here the sodium-potassium pumps do not function properly; the channels leak too much potassium and water, magnesium and oxygen out from the neuron. If these ions cause imbalance, trouble ensues. Even a small, unnecessary increase in potassium outside the cell can lead to seizures and by association to migraines.
It’s All About the Ions
So, beneath the vascular and non-vascular definitions of migraine, the neurotransmitter imbalances and the hyper-excitability of neurons in the certain brain regions associated with migraine, are simple variations in ionic balance, responsible for the onset of migraine and the possibility of vasoconstriction or relaxation changes as a consequence. Too much or too little of one or more ions, evokes changes in brain’s electrical activity that can lead to migraines or seizures. Where in the brain those changes occur determines the type of symptoms a migraineur experiences. For example, with aura migraine the anatomical initiating migraine location is the visual cortex. The migraineur sees the aura with eyes also closed. So what the migraineurs sees is happening inside the brain and not outside. The visual cortex’s function is to translate the light signals it receives into meaningful images of objects. The CSD is an electric storm that the visual cortex interprets as aura. The aura usually starts with a blind spot. It is my belief that the blind spot represents the region of neurons that is the cause of the migraine; the depolarized region that the CSD is trying to activate.
Concluding Remarks
The overall neuron-behavior is very complex but today we can say with a high degree of conviction that:
- Migraines are caused by malfunctioning neurons as a result of ion imbalances.
- Ion imbalance can be visualized by regions of depolarization.
- Depolarized regions demonstrate the anatomy of the disturbance.
- Hydration and maintaining proper ionic balance (correcting salt deficiency, magnesium deficiency, potassium excess or deficiency) is important for migraineurs since the slightest ionic imbalance can cause a migraine.
From my perspective, I am glad to see the most recent attempts at understanding physiological problems in the brain behind the migraine. This is a very important shift in migraine research – looking beyond the symptoms for a cause. Nevertheless, I am still looking for answers. How does the ion balance become so disturbed that it initiates a migraine? Why does this happen for some folks and not others? Those are the questions, researchers and clinicians need to address. My theory is that the depolarized regions of the brain result from disturbances in homeostasis and ion balance which are precipitated by dietary deficiencies. We need to determine the proper amounts of each mineral and micronutrient required for the well-functioning brain to reduce migraine.
Sources:
- Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. Martin Lauritzen, Jens Peter Dreier, Martin Fabricius, Jed A Hartings, Rudolf Graf, and Anthony John Strong; J Cereb Blood Flow Metab. Jan 2011; 31(1): 17–35. Published online Nov 3, 2010. doi: 10.1038/jcbfm.2010.191 PMCID: PMC3049472
- Cortical spreading depression as a target for anti-migraine agents. Cinzia Costa, Alessandro Tozzi, Innocenzo Rainero, Letizia Maria Cupini, Paolo Calabresi, Cenk Ayata and Paola Sarchielli1; Costa et al. The Journal of Headache and Pain 2013, 14:62
- Interpreting fMRI data: maps, modules and dimensions. Hans P. Op de Beeck, Johannes Haushofer & Nancy G. Kanwisher Nature Reviews Neuroscience 9, 123-135 (February 2008)
- Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Hadjikhani N1, Sanchez Del Rio M, Wu O, Schwartz D, Bakker D, Fischl B, Kwong KK, Cutrer FM, Rosen BR, Tootell RB, Sorensen AG, Moskowitz MA. Proc Natl Acad Sci U S A. 2001 Apr 10;98(8):4687-92. Epub 2001 Apr 3.
- Unification of Neuronal Spikes, Seizures, and Spreading Depression. Yina Wei, Ghanim Ullah, and Steven J. Schiff ; The Journal of Neuroscience, 27 August 2014, 34(35): 11733-11743; doi: 10.1523/JNEUROSCI.0516-14.2014












Angela,
Love your work on all this, but of course research findings change every day.
How then does this:
“The most recent theory about migraines involves the aberrant electrical discharges associated with migraine and a phenomenon called cortical spreading depression,”
from 2014 (https://www.hormonesmatter.com/anatomy-migraine/)
stand up to this:
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-282X2015000800714
from 2015?
They propose that
Hi Rich,
Thank you for your comment. I read the article and found it a bit inconsistent, jumping from mouse to rabbit to humans. While I totally agree that science evolves, and I also keep up with new findings as much as possible, I did not find this particular article a challenge to the current CSD (cortical spreading depression) hypothesis at all.
The researchers in this article used Transcranial magnetic stimulation, which actually activate certain brain regions and doesn’t just “listen in” as fMRIs do. In fact, it is used for treatment purposes to deliver a particular frequency of electrical stimulation to specific brain regions for therapeutic reasons. Thus since it changes the molecular and chemical nature of the ionic flow in the brain by its very nature, it is not a placebo whose consequence can be in any way removed from the findings.
I do not see the use of this method particularly useful albeit certainly cheaper and easier to get subjects to volunteer for an experiment that does not involve having to crawl into a loud machine in the middle of a migraine and look at specific objects they are shown in that claustrophobic place within an fMRI machine. While usually simpler is often better, in this case it is not, since the data they received is not “pure” as a result of the interference by the machine they used to check what was happening.
Thanks for your link to the article. It was an interesting read.
Angela
I just want to thank you for this article. I was having trouble with cortical spreading depression a few years back, and I found it absolutely impossible to get any doctor to take it seriously. I had independently determined that I could (maybe) treat it by improving my diet and conditioning my CNS with a beginner strength training program (though looking back, that seems kind of risky). That led to some improvement, but I still suffer from light sensitivity and (much milder than before) scintillating scotoma from time to time. You’ve given me another way to think about this problem so that I can at least try to correlate it with electrolyte imbalances or inconsistent salt intake. It seems that much more is known about this condition than previously, so thank you for making this information available.
Completely as an aside, this all seems like it could shed some light on why many people believe MSG triggers their migraines.
Thank you JS. I am glad you found that the explanation in this article clarified and supported your theory. My summary here of the cortical spreading depression and other findings are single-point findings – meaning if you put all of the researchers working on each little sub-topic on migraine into one room, they would not know that they are looking at the same problem from different angles. I know it is not funny at all but researchers working on little bits and parts of the problem do not see the big picture. It takes an outside researcher to see what the many within are achieving.
I summarized my findings based on all literature and what I found in my migraine group in an academic journal article that is publishing tomorrow (December 1st) in the Journal of Mental Health in Family Medicine. It is titled “Migraine Cause and Treatment” by Angela A. Stanton. You will find all that is here and more, completely clarifying all research available showing by live examples of 650 members in my migraine group (on Facebook) how the statistics completely match up to one theory that I wrote about in my book two years ago, which is now used by thousands.
Now many thousands of people are migraine free and can provide full support for the many researchers who did not even know how important their work was–starting with a paper published in 1951 that accidentally measured sodium in the urine of migraineurs and non-migraineurs. They had no idea of the importance of their findings or what it meant, for that matter.
If you have the chance, read the article–it is open access–and though they may move it by tomorrow into a different bin, as of now under “in press” it can be found here: http://www.mhfmjournal.com/abstract/migraine-cause-and-treatment-0.html
Best of luck to you and hope you will recover easier now that you know you are right and that in fact science supports your thoughts. 🙂
Best wishes,
Angela
Totally agree Lisa! While some drugs do it kind of behind the scenes, like in the case of fluoroquinolones, some actually flaunt it and those are typically the drugs given for migraines. Many reduce electrical activity in the brain or play with the sodium-potassium pumps, or reduce calcium channel activity. These can completely block all hydration efforts until the drug is taken! So the best way to get rid of migraines for those who take migraine drugs is to also get rid of these drugs at the same time, slowly by tapering off.
Of course this is not possible with antibiotics like the fluoroquinolone class of drugs since many people permanently get hurt by them. Since many fluoroquinolone drugs stay harmful in their effects even years after being taken, those who got hurt or will still get hurt face a hard challenge.
Thank you for the interesting article!!
Many pharmaceuticals, including but not limited to fluoroquinolones, mess up intracellular mineral homeostasis. If a drug depletes intracellular magnesium, all sorts of bad health outcomes result. I suspect that both pharmaceuticals and diet play a role in messing up mineral and ion homeostasis in cells to the point that migraines result.