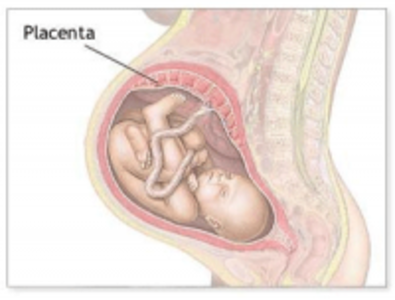
The placenta plays an important role in endocrine functioning during pregnancy. The hormones contained within the placenta at the time of parturition may still be beneficial to mothers during their postpartum recovery. As such, an entire industry has sprung up around placental encapsulation and the subsequent ingestion of these capsules. Preliminary research is beginning to identify the hormones and other substances contained within the placenta and determine what health affects ingestion of placental pills may elicit. This article reviews some of the research in placentophagy.
Currently known hormones, vitamins and minerals found in placental tissue:
- Corticotrophin-releasing hormone (CRH) and Cortisol
- Progesterone
- Estrogens (estrone, estradiol and estriol)
- Endorphins
- Thyroid-Releasing hormone (TRH), thyroid-stimulating immunoglobulines and ultimately Thyroxine (T4)
- Oxytocin
- Prolactin and Human Placental Lactagon (hPL)
- Leuteinizing hormone (LH)
- Human Chorionic gonadotropin (hCG)
Other relevant components:
- Placental Opioid-Enhancing Factor (POEF)
- Iron
- Vitamin B6
Many of these hormones have been linked to the onset of Postpartum Depression in women. For example, progesterone plays a key role during pregnancy. Recent studies have shown that progesterone has an MAO-inhibiting effect during pregnancy, having a similar impact as some anti-anxiety medications (Ford 1996). Therapies that introduce progesterone and estradiol back into the system have been helpful in relieving depressive symptoms (Arpels 1996). Endorphins are the “feel good” neurotransmitters. By increasing estradiol and progesterone, the level of endorphins is also increased (Ford 1996). The levels of estradiol and estriol (the primary estrogens of pregnancy) and progesterone in a woman’s system drop precipitously after birth, reaching pre-pregnancy levels by day five postpartum (Hendrick 1998).
CRH and Cortisol are stress-relieving hormones. CRH is secreted by the placenta in high levels during the last trimester of pregnancy. These levels drop dramatically after birth, and one study found that those women with the lowest levels of CRH also experienced depressive symptoms (Chrousos 1995).
Thyroid-Releasing Hormone and Thyroxine are implicated in a variety of mental health disorders. Women with an abnormality in their hypothalamic-pituitary-thyroid axis show an increased tendency toward panic attacks, suicide, agitation, psychosis and bi-polar disorders, among other issues. The thyroid has such an impact because these hormones interact with brain messengers that influence mood and emotions (Ford 1996). Postpartum women have slightly more elevated rates of thyroid dysfunction than the general female population (Hendrick 1998).
Fatigue levels may predict the development of Postpartum Depression (Corwin E 2005). Iron, or rather, iron deficiency, has been strongly linked to fatigue. Even slight iron supplementation can help relieve the symptoms of fatigue (Verdon 2003). Some suggest that since increasing a mother’s iron stores can help relieve fatigue, it may also reduce the risk factors for developing Postpartum Depression later.
Since the placenta is known to contain many of the components that a postpartum woman is lacking following parturition, many believe that by ingesting the placenta postpartum women can re-balance their systems more quickly. Placental encapsulation, the process by which the placenta is dried and encapsulated for future ingestion, has become popular among celebrities and women seeking more holistic birth experiences.
The research on the purported health benefits has only recently begun, although placental encapsulation and ingestion has been used in Chinese Medicine for hundreds of years. One of the primary questions to be answered is whether the processing of the placenta would ruin or eliminate some of the hormones, vitamins and minerals present in the placenta. Some preliminary research, to be published out of the University of Nevada, Las Vegas found that many of the compounds present pre-processing remained post-processing. The study analyzed several components present in placenta before any type of preparation, and after the steaming and dehydration that is common in converting the placenta into capsule form. The results demonstrated that while some components are reduced in the dried state, many components do still remain. In fact, the research has shown that the iron content, in particular, is even more highly concentrated after dehydration (Benysheck 2012).
There have been few negative responses from women following ingestion of the placenta. Recently, Nancy Redd, a NYT writer, reported mood related, ill-effects after consuming placental pills.
In another study, researchers found that most women who have ingested placenta after a birth would do so again after a subsequent pregnancy (Selander 2012).
While much research remains to be completed, the possibility that placental encapsulation and ingestion could improve postpartum recovery remains an intriguing notion.
Works Cited
Arpels, J.C. “The Female brain hypoestrogonic continuum from the pre-menstrual syndrome to menopause; A hypothesis and review of supporting data.” Journal of Reproductive Medicine 41 (1996): 633-639.
Benysheck, Young, Selander, Cantor. “Eating the placenta: A comparison of select hormones and nutrients in unprepared placental tissue and placenta prepared for encapsulation.” Ecology of Food and Nutrition, in press.
Selander, Cantor, Young, Benysheck.”Human maternal placentophagy: a pilot survey of self-reported motivations and experiences associated with placenta consumption.” Ecology of Food and Nutrition, in press.
Lucine Medical Disclaimer: All material on this website is provided for your information only and may not be construed as, nor should it be a substitute for, professional medical advice. To read more about our health policy see Terms of Use.
About the Author: Jodi Selander started researching placentophagy in 2005 during her second pregnancy. She found substantial information documenting the benefits it offered. Having dealt with depression for many years, Jodi had many risk factors for developing postpartum depression. With a B.S. in Psychology, she understood the devastating effects depression could have on women and their families. As a natural health enthusiast, she wanted an alternative to pharmaceuticals that might help avoid those issues. To learn more about Jodi, click HERE.