“If sexuality is one dimension of our ability to live passionately in the world then in cutting off our sexual feelings we diminish our overall power to feel, know, and value deeply.” –Judith Plaskow
This quote raises an interesting question. If owning our sexuality gives us power, then who benefits from limiting that power? And why is limiting that power an acceptable side effect of hormonal contraception?
During the Nelson Pill Hearings, Dr. M. James Whitelaw testified (page 6015): “How many adult males would be willing to take an oral contraceptive faithfully if they were told that instead of a possible 50-plus adverse side reactions only one remained, that being the possible loss of sex drive and libido? [Laughter]”
What is the implication here? Women can be denied their full sexual capability but the idea of men suffering the same is laughable? Holly Grigg-Spall speaks to that in her book Sweetening the Pill (page 50):
“The pill’s impact on the libido has been publicized but it is generally dismissed with humor. The libido is seen as distinct from women’s emotional and physical health, whereas with men it is linked. The female sex drive is not celebrated or seen as essential to her femininity or sexuality… Research that indicates that lowered libido is experienced by a large number of women on the pill is undercut by the cultural assumption that most women have little real interest in sex regardless of this drug.”
Sexy But Not Sexual
And she’s right. Women are constantly told to be sexy but not sexual. It would seem that hormonal birth control would provide exactly that type of woman. One who could have sex without the consequence of getting pregnant, therefore highly desirable to men; but one who could not fully embrace the power of her own sexuality due to a medication-induced lack of libido. Is this really what we want? A society of women that are physically available for sex but completely disconnected from the powers of her own sexuality? Again I will ask, who benefits from keeping women in that robot-like state?
“The quality of a woman’s sex life, unlike that of a man’s, does not seem to concern the drug companies or the (male) research establishment… Women who reported changes in their sex drive often heard that old refrain: ‘It’s all in your head.’ But the male sex drive is considered so important by the drug companies that it is always studied in conjunction with new male contraceptives, just as it is almost always mentioned in arguments against the condom.” –Barbara Seamen in The Doctors’ Case Against the Pill
It’s true. We hear the argument that condoms lessen sensation during sex. But for whom? Men. Yet for women who use hormonal birth control, low libido and loss of sensation during sex are some of the least dangerous side effects they can expect. Heather Corinna put it so well in her article “Love the Glove” that even Grigg-Spall quoted her:
“If we’re going to talk about condoms changing how sex feels, we need to remember that something like the pill does too, and, unlike condoms, it changes how a woman feels all the time, both during and outside of sex… Other methods of contraception can cause pain and cramping, unpredictable bleeding, urinary tract infections, depression and a whole host of unpleasant side effects. Condoms are the LEAST intrusive and demanding of all methods of contraception, even though some guys talk about them — without considering this perspective — like they’re the most. If guys could feel what life can be like on the pill, use a cervical barrier or get a Depo shot, they’d easily see condoms for the cakewalk they are.”
It’s not just the pill that is damaging to women. As Grigg-Spall explains, Depo Provera (“the shot”) is specifically used to decrease sex drive in sex offender rehabilitation programs. There is something seriously wrong when a birth control option offered to women is the exact same medication used as pharmaceutical castration for sex offenders.
FSD – Female Sexual Dysfunction or Female Sexuality Discouraged?
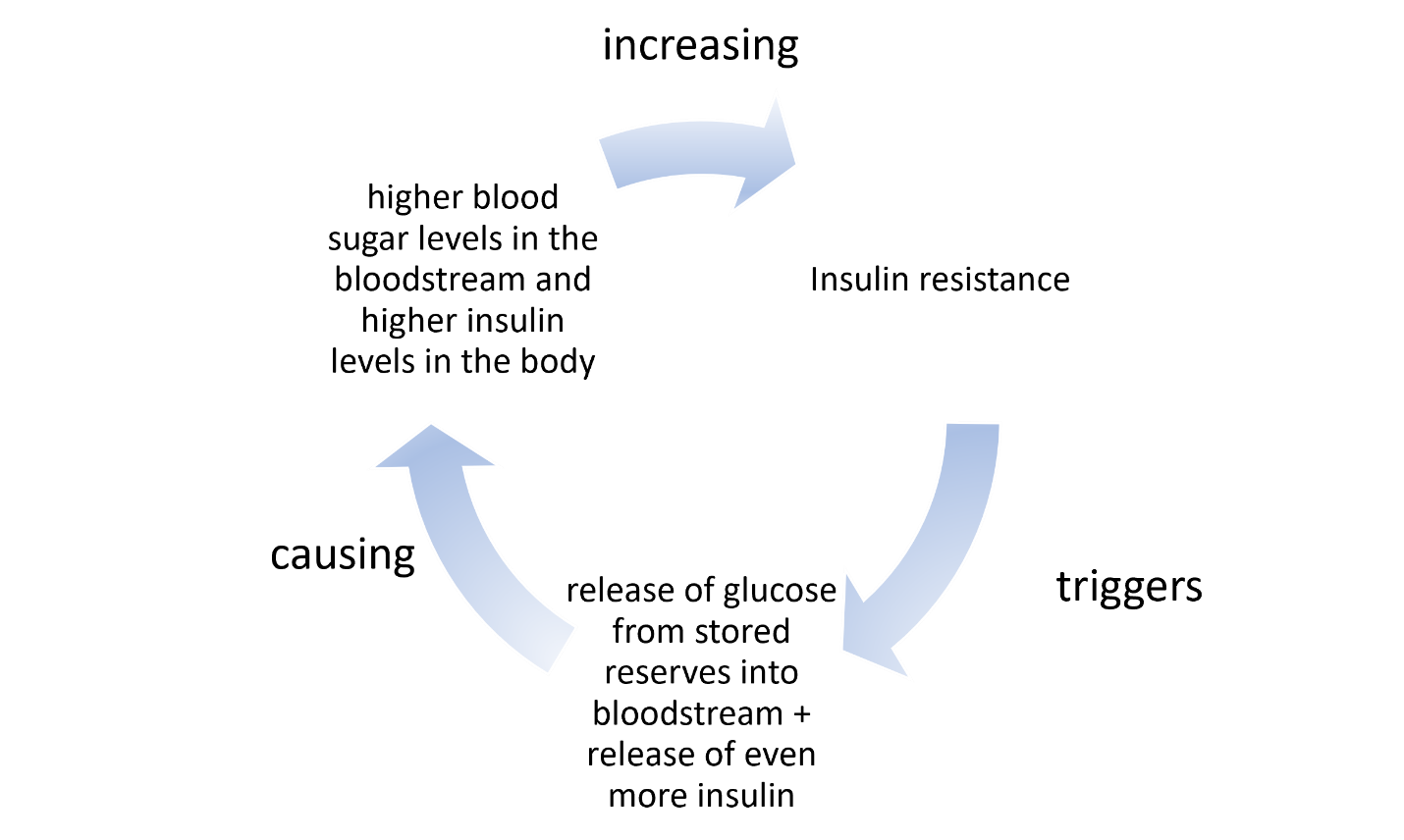
According to a study of female German medical students published today in The Journal of Sexual Medicine, women taking non-oral and oral hormonal contraceptives were at highest risk of Female Sexual Dysfunction (FSD). Interestingly, women using non-hormonal contraceptives were at lowest risk for FSD, more than women not using any contraceptive.
“Sexual problems can have a negative impact on both quality of life and emotional well-being, regardless of age,” said researcher Dr. Lisa-Maria Wallwiener of the University of Heidelberg, Germany. “FSD is a very common disorder, with an estimated prevalence of about two in five women having at least one sexual dysfunction, and the most common complaint appearing to be low desire.”
Side Effects – Affecting More Than Just the Patient
Why is this okay? Why do we accept this? If a woman is experiencing sexual dysfunction, it not only affects her but it affects her partner as well.
Dr. Philip Ball testified about this very problem at the Nelson Pill Hearings back in 1970 (page 6493): These unhappily newly married women do not know if it is the wrong man, the wrong town, the wrong job, the wrong year, the wrong apartment, or yet something else, when it is really many times the wrong pill.
And he’s not incorrect. Research now shows that taking birth control pills affects women’s taste in men. According to this article from the Scientific American, women on the pill seem to prefer men who are genetically similar to themselves.
“Women who start or stop taking the pill, then, may be in for some relationship problems. A study published last year in Psychological Science found that women paired with MHC-similar men are less sexually satisfied and more likely to cheat on their partners than women paired with MHC-dissimilar men. So a woman on the pill, for example, might be more likely to start dating a MHC-similar man, but he could ultimately leave her less sexually satisfied. Then if she goes off the pill during the relationship, the accompanying hormonal changes will draw her even more strongly toward more MHC-dissimilar men. These immune genes may have a “powerful effect in terms of how well relationships are cemented,” says University of Liverpool psychologist Craig Roberts, co-author of the August paper.”
How any of this is connected to relationship issues, divorce rate, infertility, one can only speculate. But it’s clear that the sexual side effects caused by hormonal contraception are no laughing matter.
Sex is a big part of life. The ability to connect with each other and derive great pleasure from sex is not just a perk of being a human. It is our birthright. And to deny that birthright is to limit our power as women. That’s not what I consider an “acceptable side effect.”
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Pana Koutloumpasis from Pixabay.
This article was published originally on July 14, 2016.