Dr. Marrs and I are very much on the same plane of thinking. We both believe that much of the illness in America is not being recognized for what it really represents, hence the publication of our book: Thiamine Deficiency Disease, Dysautonomia and High Calorie Malnutrition. I want to give you an illustration of a typical situation where the patient is falling through the cracks of modern medicine. I live in a retirement home and one of my friends who is resident here told me the following story, believing that his medical history was a reflection of how well he had been treated.
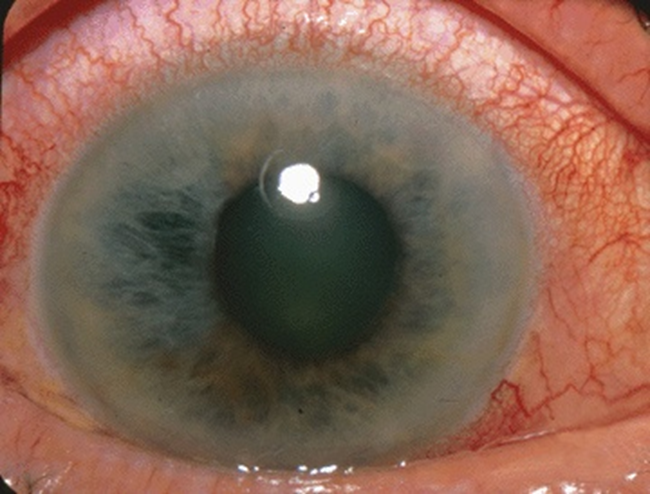
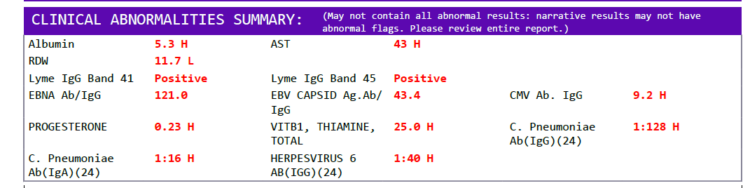
Open Angle Glaucoma: A Marker of Autonomic System Dysfunction
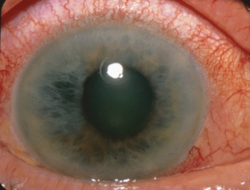
His story begins in his forties with a burgeoning glaucoma in the left eye. He told me that the surgeon had to make a cut in his eye to let the fluid out and he later required a corneal transplant. At the time he was smoking a pack a day of cigarettes. He continued by telling me that he periodically had cardiac palpitations and in his fifties he had cardiac bypass surgery and was being treated with aspirin. He still experiences heart palpitations. At present, he has periods where he is unable to catch his breath, sometimes for half an hour or so. As he was telling me his story, I could clearly see that all of these events might easily be put together with one underlying cause. Ophthalmologists (eye specialists) know perfectly well that one type of glaucoma known as “open angle” is not a disease of the eye. It is a disease of the autonomic nervous system (ANS), so let me try to explain this.
The eye-ball is filled with fluid that has entry and exit portals, allowing for the circulation of nutrient bearing fluid throughout the eye. Entrance and exit are controlled by a branch of the ANS. If the exit mechanism fails, the fluid cannot leave the eye and the pressure builds up. The exit is in an angle representing the detailed way in which the eyeball is constructed, hence the termination “open angle”. The key to relieving the fluid buildup is by fixing the neurological control of the entrance and exit of fluid.
The trouble with this is that the pressure can build up slowly and even the vaguest eye symptoms are unlikely. Even when visual limits are first noted, the disease is usually quite advanced. Increased blood pressure or family history of glaucoma may be an indication for an eye examination on a regular basis. The next thing to be understood is that the ANS is not symmetrical. In other words the right half of the body is controlled differently from the left half, thus explaining why the glaucoma can be in only one eye. In my view, in an ideal medical situation, the eye doctor should have advised the patient of the underlying cause and referred him for further evaluation. The patient should have been informed that the “pack a day” of cigarettes was the underlying cause of the glaucoma. He is unlikely to have suspected the connection.
Other Symptoms of Autonomic Disruption: Sleep Apnea, Dyspnea and Heart Palpitations
Evidence for the ANS association has been shown by the fact that sleep apnea (repeated temporary cessation of automatic breathing in sleep), surprisingly common in the United States, is prevalent in primary open-angle glaucoma patients. Although this would be a potential clue for an eye examination, there was no history of sleep apnea indicated by my friend. This disease develops because of defective control mechanisms in the brainstem and automatic breathing, particularly necessary in sleep, is mediated through the ANS. The complaint of cardiac palpitations also indicates abnormal activity of the ANS, because the speed and regularity of the heart is controlled by this system. Finally, his difficulty in breathing with the technical name of dyspnea is typical of heart and lung disease. His previous history of heart palpitations suggests that this is heart-related. I would suggest that his health is in a precarious state and I think that he might wind up eventually by being treated with nasally administered oxygen, as I see repeatedly in other elderly residents. I often wonder whether the oxygen is really giving benefit if the catalysts that enable cells to use it are in insufficient supply, because they are never given a thought.
Disparate Symptoms within the Framework of Dysautonomia
Most people know that we have two nervous systems. One is known as voluntary and the other that takes care of all automatic mechanisms in the body, is called the ANS. This is the nervous system with which we are concerned here. The brain may be thought of as having two primary sections. The upper part thinks while the lower part automates by signals to and from all the organs in the body through the wiring of the ANS and a bunch of glands known as the endocrine system. Another illustration of asymmetry, as indicated in this case of glaucoma, is the fact that nerves from the ANS deliver a different signal to the heart from the right side of the body versus the left side. One controls the strength of contraction of the heart while the other controls the speed at which it beats. Therefore, it is not too difficult to understand that heart palpitations are a function of this nervous control and that their cause is the same one that gave rise to glaucoma, faulty action of the ANS. Finally, the difficulty in breathing is because of defective metabolism in the brainstem where automatic breathing is controlled. That is why glaucoma and sleep apnea sometimes occur together as we have stated.
Why the Autonomic System Becomes Disturbed? Poor Oxidative Metabolism
The lower part of the brain, known as the limbic system, is a complex of cells that come together in the operation of the ANS and endocrine system. The metabolism of these cells is inordinately dependent on a high rate of oxygen utilization. Because of this, they are very sensitive to thiamine deficiency, resulting in what is sometimes referred to as brain pseudohypoxia (false lack of oxygen). The lack of energy in these cells produces abnormal function in the ANS.
The toxic effect of smoking results in slowly producing damage in oxidative metabolism. This may give rise only to minor changes in mental or physical fitness, sometimes for years, but the metabolic inefficiency eventually affects the ANS, often initiating serious disease, as in this case. Although smoking is generally thought of as the commonest cause of lung cancer, it has a much wider danger of triggering virtually any disease because of its role in reducing cellular energy. There is circumstantial evidence that many, if not all, diseases are the result of oxidative dysfunction. Zbinden published a paper in which he found 696 papers that described treatment of 242 different diseases, other than beriberi, with thiamine, providing a variable degree of success.
We can now see why the patient described above had a series of events that could be ascribed to an underlying cause in common, inefficient oxidation. In fact, the symptoms of beriberi, none of which are pathognomonic (strong indicators of that disease exclusively), are so prolific that it can be looked at as the great imitator of disease. Chronic fatigue, heart palpitations, insomnia, abdominal bloating, constipation, panic attacks and many other symptoms, so often regarded erroneously as psychological or referred to as Chronic Fatigue Syndrome are common in America today. The official medical denial of it as an acceptable solution leave the unfortunate patient in limbo without the necessary, relatively simple treatment that is so effective.
The Problems with Compartmentalized Medicine
It seems to me that the patient that I have described represents a failure of perspective in modern medicine. The glaucoma is treated as an eye disease and changes in heart function are seen as diseases of the heart, whereas the two have an identical underlying cause, chiefly in the brain. The patient can be seen as slipping through the cracks in perspective and it carries with it a serious indictment of the present medical model. The surgical approach to the glaucoma was unavoidable and saved the patient’s eye. We know that that kind of glaucoma can build up slowly without the patient being aware.
My point is this: I would be willing to bet that the patient had other trivial symptoms at the time of his glaucoma that would be a reflection of abnormal ANS activity. They could have been so trivial that they weren’t even mentioned to the physician and long forgotten by the patient when serious disease made its appearance. Although the glaucoma could not have been predicted even under those circumstances, at least it would not have been a surprise to the ophthalmologist. In an ideal doctor/patient relationship, the ophthalmologist would be aware of the ANS connection and refer the patient to a colleague who understands this underlying cause. The later development of heart palpitations might have been seen differently as dysfunction in the ANS. Modern heart disease and thiamine deficiency have recently been connected.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
“Photo showing acute angle-closure glaucoma which is a sudden elevation in intraocular pressure that occurs when the iris blocks the eye’s drainage channel—the trabecular meshwork.”
Image credit: Jonathan Trobe, M.D., CC BY 3.0, via Wikimedia Commons.
This article was published originally on August 22, 2019.