Symptoms of pain related to the bladder, urinary urgency and/or frequency affect up to 12 million Americans and can range from uncomfortable
MoreFour years ago, when the heavy period bleeding which I’d had since adolescence suddenly became much worse, I never would have predicted
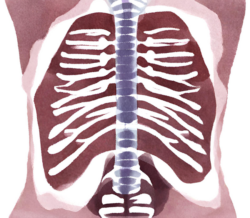
MoreThoracic Endometriosis
Endometriosis is a common disease, affecting up to 10% of women. It is characterized by the presence of tissue similar to the
MoreRestless Legs Syndrome
Restless Legs Syndrome (RLS), also called Willis-Ekbom disease, is both a neurological and a sleep disorder that is common, but under-recognized. It
MoreCyclic vomiting syndrome (CVS) is a debilitating disease characterized by episodes of severe nausea and persistent vomiting interspersed with periods of wellness.
MoreIn my work with The Endometriosis Network Canada, I have heard many women say that their doctors told them that if their pain
MoreFatigue is a very common complaint, reported to general practice doctors up to 25 percent of office visits. The incidence of fatigue
MoreInaccurate theories about how and why endometriosis develops are widely accepted by medical practitioners, despite much evidence against them. Acceptance of these
More