I was prompted to write this article because of the recent bad news that Kelly Preston had died of breast cancer at 57. She leaves behind a son who is just 9 – and a grieving family. She is just two years younger than I am.
I find myself sitting here, and wondering: did she try to eat “extra healthy” to get well, particularly since her diagnosis with breast cancer? Did she – like me – end up eating a very high oxalate diet in order to be the best older mom she could be? Before I learned about the impact of oxalate, my diet was simply sky high in oxalates. I shudder to think now. Was oxalate on her radar?
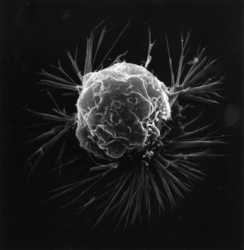
I’m going to make a bold statement: oxalate should be on every woman’s radar. Here is the main reason why – oxalate induces breast cancer:
“We found that the chronic exposure of breast epithelial cells to oxalate promotes the transformation of breast cells from normal to tumor cells, inducing the expression of a proto-oncogen as c-fos and proliferation in breast cancer cells. Furthermore, oxalate has a carcinogenic effect when injected into the mammary fatpad in mice, generating highly malignant and undifferentiated tumors with the characteristics of fibrosarcomas of the breast. As oxalates seem to promote these differences, it is expected that a significant reduction in the incidence of breast cancer tumors could be reached if it were possible to control oxalate production or its carcinogenic activity.”
That’s pretty definitive, but when you look into the research, it has taken some time for the understanding of oxalate and breast cancer to develop.
Oxalate and Breast Cancer: The Research
In 2003, researchers noted that women with “casting type” microcalcifications could have poor prognosis, depending on the type of cancer. Another study done in 2004 showed that casting type calcifications were associated with increased risk of death when patients had small invasive breast carcinoma. Most casting type microcalcifications are apatite-based, and so oxalate seemed to be off the hook.
By 2005, research showed that women with calcium oxalate calcifications could be associated with some types of cancer, but it was believed that the presence of oxalate was still mostly benign.
But by 2015, when researchers first tied oxalate and breast cancer together, the tide was turning.
In 2019, there was a study done indicating that, in the presence of calcium oxalate and activated monocytes, breast cells undergo a transition. This transition suggests that micro calcifications are implicated in both breast cancer occurrence and progression. Biopsies were collected from women showed that outcomes were more likely to be negative, regardless of whether the initial biopsy was benign or cancerous, in the presence of calcium oxalate calcifications.
Another important 2019 study was done to follow up on the medical observations of doctors that both hydroxyapatite and oxalate based micro calcifications are frequently observed in breast cancer tissues. The concerning conclusions of the research included both that DNA undergoes significant structural distortion when adsorbed into calcium oxalate and, that the DNA itself destabilizes when encapsulated into calcium oxalate nanopores. Nanopores may be formed when very small holes develop in a microcrystal.
Reducing Dietary Oxalate
The aforementioned research leaves us with good reason to look at oxalate and be concerned. Obviously, more research will be needed to be definitive about the level of risk that oxalate poses. This does not mean that we have to wait to take action. If you are a woman who wants to reduce your risk of oxalate-induced breast cancer, consider reducing oxalate in your diet.
Reducing dietary oxalate may be more complicated than it might seem at first glance. Oxalate values vary even between different types of the same plant food, therefore, it can take time to understand where the oxalate is in your diet, and adjust as works best for you. However, some of the highest oxalate foods are those that we consider healthy and often consume in large quantities when dieting especially if following juicing type type diet. High oxalate foods include: spinach, beets and their greens, Swiss chard, sweet potatoes, plantain, rhubarb, nopal, star fruit, Indian gooseberry, almonds and most nuts, black beans (and many other legumes), turmeric, cumin, cinnamon (and a number of spices), teff, amaranth, buckwheat, wheat bran (and other grains), as well as (unfortunately) chocolate, cocoa powder and carob. For more information on high oxalate foods, click here.
Another small step that is oxalate related could be the addition of walnut oil in your diet. It turns out that walnuts included in the diet can inhibit pathways that promote cell proliferation in breast cancers. The original research had women consuming two ounces of walnuts per day. The challenge is that walnuts are actually a very high oxalate food, with walnuts having about 40 mg of oxalate in two ounces. In this case, it may be possible that you could consume walnut oil as an alternative, and may still obtain the therapeutic effect. However, note that the study was done on a very small group of women, and so more research is absolutely needed.
While the research on the relationship between high oxalate diets and breast cancer is just beginning to be recognized, there is huge body of work demonstrating that dietary oxalates negatively impact health via bioaccumulation. If you suffer from unexplained chronic health conditions, it might be worth it to consider reducing your dietary oxalate.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
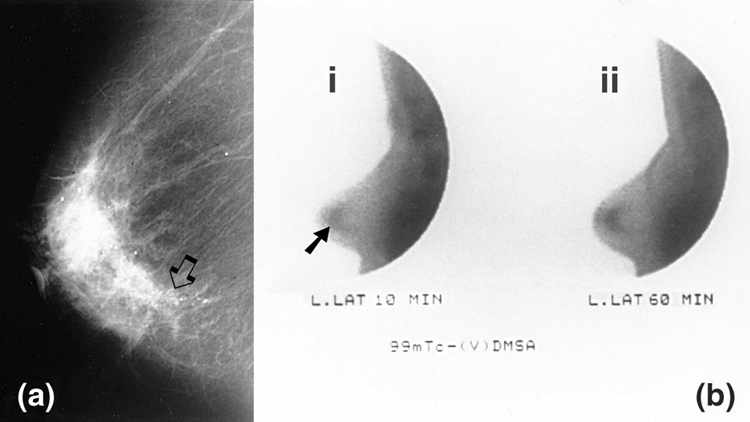
Image credit: Vassilios Papantoniou, Spyridon Tsiouris, Ekaterini Mainta, Varvara Valotassiou, Michael Souvatzoglou, Maria Sotiropoulou, Lydia Nakopoulou, Dimitrios Lazaris, Androniki Louvrou, Maria Melissinou, Artemis Tzannetaki, Ioannis Pirmettis, John Koutsikos and Cherry Zerva, CC BY 2.0, via Wikimedia Commons
This article was published originally on July 29, 2020.










Hi, Wayne! Thanks for your kind words about my article. Much appreciated!
While I agree that endogenous oxalate is a definite hazard and more associated with oxalosis, I have been working with two clients recently who both have breast cancer and neither are endogenous oxalate producers (based on their tests). I’ve also been reading about cases of oxalosis that have been the result of dietary changes that are relatively easy in today’s world. Here’s a great example, where all that happened is the person decided cashews would be very healthy, and started to consume 3 1/2 to 5 ounces of cashews a day. (Very easily done.) The results were pretty startling. https://pubmed.ncbi.nlm.nih.gov/27956392/
I think it can become too easy to look for a complicated answer, when the simple answer may be that high dietary oxalate could be setting us up for all kinds of things. While I can’t say for certain, what if high dietary oxalate is the original “insult” to our health that sets us up for other things? So it’s been something I’m thinking about.
As a result of that thinking, I totally agree that a low oxalate diet alone may not be the single and sufficient answer. If we have developed some level of oxalosis from diet (or for any other reason), we definitely will have other “fish to fry” as the expression goes. But if we can dodge that initial bullet, I’m hoping some people may avoid much worse things over the longer haul.
Thanks for coming to comment, and giving other readers something to think about.
Excellent article. I only would add that endogenous oxalate, not dietary oxalate, is attributed to most oxalosis. Reducing fungal infections in the liver and elsewhere (aspergillus niger) by taking Berberine, Biotin and avoiding high fungus foods (mushrooms, blue cheese, peanut butter and nuts, spoiled processed meats) is necessary to control oxalates. Oxalosis is a metabolism problem; we both make non-nutritional metabolites (like oxalate, uric-acid and phosphate crystals) in our body when we do not digest food sufficiently; and we can also consume high amounts of excessively high oxalate foods. But the low ox diet alone may not be enough.
Hi Wayne,
Curious what you mean by reducing fungal infections elsewhere (aspergillus niger)? Specifically what you mean by your reference to aspergillus niger?
Thanks,
Debbie
oxalates dont cause as much damage as you may think since most people cook their veges. Most breast cancer is actually caused by root canals and amalgam fillings . I gurantee most women who have breast cancer have 1 of those.
I totally agree with you.. I had one amalgam break off and then the mercury went into my face after them drilling it out.. 3 different spots. My last visit I asked them and they said sometimes you get mercury tattoos.. It took me a few years but I did get it out, but it is an ongoing problem. I will not go near Dentists again unless I could see a Biological Dentist. I would, but I am on a budget and with how things are going its getting worse.
Healing naturally.. No Surgery.. No Drugs
My question does anyone know which type of breast cancer is connected to oxalates.
I wrote a letter to Lobular breast cancer alliance asking them and never got a response and you can’t be in a study unless you have surgery.. They just want money..
I don’t believe healing should cost MILIONS! I am going on 4 years diagnosis and they said I would be gone July 2020, well I am still here going stronger than ever! NO FEAR
Here is the link for the original study that I looked at. I’d have to re-read the full text, but not sure that they stated a type of cancer; but there is a link to microcalcifications. https://pubmed.ncbi.nlm.nih.gov/26493452/
What is your comment based on? I find it rather irresponsible to say such a thing or at least word it in such a way. I’ve had 3 women in my family go thru breast cancer among countless friends and acquaintances and almost none of them have mercury issues and I only know this because they come to me for help knowing I like to study these topics in hopes of helping people with their health. I think that Oxalates are a very real issue and dismissing them in such a way could prevent people from making sound decisions to better their health. I know they were a massive factor in my health journey and continue to be, especially since they can take years or even decades to overcome. Maybe you could share a bit more of how you’ve come to this conclusion?
I poisoned myself with oxlates and have done a lot of research. Unfortunately oxalates can’t be cooked out of food. If you boil your veggies and throw out the water, you can get rid of at most 10% of the oxalates. Sprouting can often liberate oxalates. And fermenting does nothing to reduce oxalate content. I agree with you about the root canals and amalgam fillings – nasty health destroying procedures.