Are you familiar with the phrase “iatrogenic illness”? An affirmative answer is more likely among the readers of this website than the public at large, but I would argue that even we (those of us who frequent this website) don’t give it the attention it deserves. In fact, if we changed the way we looked at iatrogenic illness, it could reframe the way we look at the entirety of medicine.
The Effect of Side Effects
Iatrogenic means an ailment that is actually caused by a medical examination or treatment. Perhaps the reason it receives less attention than it should lies in the fact that the classification would usually require an admission of guilt from the person most likely to identify it. Most doctors aren’t inclined to draw attention to the fact that something they did caused a new problem.
Consequently, we tend to associate iatrogenic illnesses with things like infection after a surgery, where it happens despite the medical team’s best efforts to prevent it. And, the only time we weigh the iatrogenic effect of pharmaceuticals being administered comes in extreme cases, like chemotherapy, where the patient and their family often weigh the quality of life versus the quantity.
However, we really should start considering the quantity of effect versus quality much sooner in life.
The Primary Effect
Think about the early development of a new drug and then consider this old phrase:
“There are no side effects, only effects.”
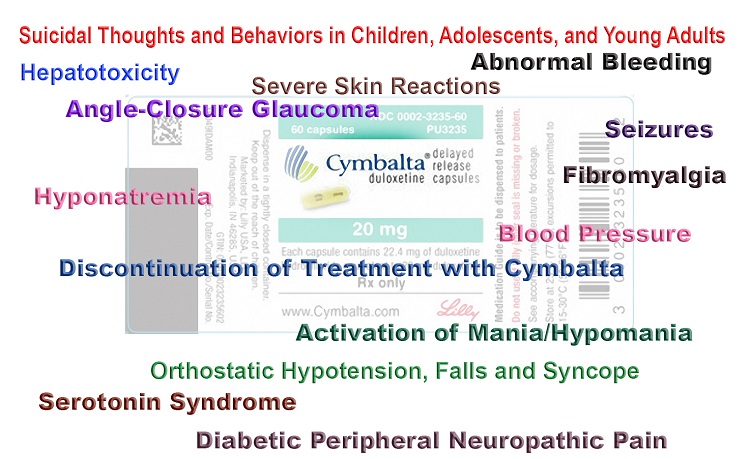
When a new drug is in development, the chemical engineers have a sense of what the desired effect will be, largely because most new drugs are variations on existing medications. But, this focus on a primary effect can lead us to discount the other effects on the body. It’s as if simply labeling an effect as a ‘side effect’ trivializes it in our minds.
What we must keep in mind is that by introducing these compounds into our bodies, we open ourselves up to the potential to experience any and all of the various effects. The doctor may give it to us to treat a specific ailment, but the reality is we’re susceptible to the entire array of effects.
Granted, these other ‘side’ effects may not happen as frequently as the ‘primary’ effect, but are drug makers still failing to give them proper attention as they weigh the benefit-to-risk simply because of how they may negatively impact marketing?
Creating a Drug Market
Let’s look at a couple of examples to see how marketing ultimately determines which is the ‘primary’ effect of a drug. We will begin with a brand so familiar it has almost become a generic term for analgesics.
In the late 1800s, an inexperienced pharmacist mistakenly sent acetanilide instead of naphthalene to a couple of French doctors who were experimenting with treatments for intestinal parasites. By chance, the doctors soon discovered the new compound reduced fever in some patients and later realized it offered some level of pain relief.
While unexpected, the ‘side’ effects were marketable. That’s why nearly 150 years later acetanilide, which metabolizes in the body to become acetaminophen, is still marketed under the brand name Tylenol, and has become synonymous with its ‘primary’ effects of pain relief and fever reduction, rather than its effect on parasite motility.
What about the other effects – the less marketable ones? Liver damage would probably fall into that category, And, despite the long history, researchers didn’t really start looking into the impact of acetaminophen toxicity on livers in both adults and children until this millennium. It makes one wonder how many people suffered severe liver damage before it caught researchers’ attention.
To some extent, the failure to notice the negative effects can be chalked up to human nature. As we look for the hook to hang our hat, we aren’t likely to notice the corner of the dresser until our little toe ultimately discovers it at a most inopportune time.
One Effect Stands Out
Drug makers aren’t completely oblivious to ‘side’ effects as they develop a new drug. In fact, they become acutely aware of secondary effects when they provide the potential for more profits.
It is a well-known story that the makers of one new drug being developed for high blood pressure and angina discovered that the drug also effectively induced erections in many of their male patients. Once they stripped away the labels of primary effect versus side effects, it probably didn’t take Pfizer’s MBAs long to recognize Viagra’s potential.
Rather than join the crowded, competitive field of blood pressure drugs, they had the opportunity to essentially create a new market catering to those suffering from impotence.
Of course, erectile dysfunction sounds much more like something that needs to be treated so they put their ad budget toward branding the ‘ailment’ as much as the new drug and it paid off in spades. Viagra managed to stay in the range of $2 billion in each year of its patent protection.
Don’t Take Your Eye Off the Ball
The drug and medical industries, which are so clearly on top of the ball when it comes to drug outcomes and profitability, have an abysmal record when it comes to drug outcomes and actual patient experience. It is precisely this focus on profits that clouds their vision, and turns side effects into new symptoms.
This is problematic with any drug, but none more so than with birth control because the patient is typically young and healthy. Plus, I can think of no other drug that is designed to be given to a healthy patient with the intent of stopping a natural process.
Given the disease-free state of so many patients who begin birth control, you would think this is one drug where it would be easy to identify an iatrogenic effect when side effects begin to arise. However, this is rarely the case, and the story of a young woman who recently contacted me provides a perfect example.
A Pattern of Side Effects
After seven years of taking birth control pills, Alexa changed over to the Mirena IUD. She began to notice facial hair growing and mentioned it to her doctor. He ran some tests and discovered her DHEA-S levels were high. A subsequent ultrasound revealed the classic string of pearls on her ovarian tissue, and she was diagnosed with PCOS.
When she questioned her birth control, the doctor insisted that she NEEDED to be on birth control or she would likely end up with endometrial cancer. She felt almost like he was using cancer to threaten her into continuing with birth control. He began to discuss other medicines she would also need to treat her condition.
But, she knew that her ovaries had been fine before starting on Mirena, and just couldn’t accept what the doctor was telling her. She searched online and found the patient information pamphlet for her IUD and learned that the documented side effects include “cysts on ovaries” and “facial hair.”
Alexa opted to take supplements to help balance her hormones and began charting her cycle after removing the IUD. Her cycle normalized quickly, her mood stabilized, and her energy rebounded.
It was the first time she began to realize how much the synthetic hormones had dragged her down over the years. She began to take inventory of all the “symptoms” that she encountered after starting birth control that might have actually been “side effects.”
Not only had the doctor recently missed that the two symptoms (facial hair, ovarian cysts) he used to diagnose PCOS were clearly listed as side effects of the contraceptive device he inserted, but she began to question previous interactions.
The IUD contributed to multiple vaginal infections, which in turn, led to several antibiotic prescriptions, but her doctor never acknowledged that the IUD could have played a role, even though these types of infections had never been a problem prior to the IUD.
She could see a pattern developing.
Then, she remembered when she first started taking The Pill at age 15. She experienced her first bouts of depression, which triggered new scripts for Paxil and then Lexapro.
Depression and anxiety represent some of the most common side effects of hormonal birth control. Yet, they are treated as mere symptoms of a new, unrelated disease by a vast majority of doctors.
A Cascade of Symptoms
I wonder how many young women have lived a similar experience? They unwittingly trade in their health for a cascade of symptoms.
When you hear a story like Alexa’s, you begin to understand why 131 million people in the US take at least one prescription drug, with the average being 4 prescriptions. We lead the world, spending $1,376 annually per capita on these drugs, nearly 50% more than our nearest competitor, Germany.
I don’t mean to insinuate that these new symptoms aren’t in fact new diseases. The subsequent effects of birth control often manifest as long-term, even chronic, new diseases. It isn’t uncommon for synthetic hormones to trigger an autoimmune disease, nor is it uncommon for depression to linger long after a woman stops taking birth control.
These long-term consequences are precisely why the next time your doctor casually hands you a prescription and you feel compelled to bite your lip and not ask the questions bouncing around in your head, ponder the phrase “iatrogenic illness” and don’t be afraid to start questioning the doctor.
After all, you will be the one living (or dying) with the consequences.

The FDA approved The Pill despite it not being proven safe. Today, it has been linked to everything from blood clots and cancer to lupus and Crohn’s disease — and still has not been proven safe.
This book explores the medical and historical disconnects that brought us to this point.
Last updated on October 21, 2023 at 9:38 pm – Image source: Amazon Affiliate Program. All statements without guarantee.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image Credit: Photo by krakenimages on Unsplash.
This article was originally published on September 26, 2022.