Survey History
A few years ago, I embarked on a massive research project involving medication adverse reactions. I launched several online studies on the drugs that were popping up on our radar screen as having the most frequent and serious side effects; side effects that were largely ignored in the medical literature. At the time, this work was unfunded and, to a large degree, remains so today (feel free to contribute to our efforts). Despite the lack of funding, I thought it was important to investigate drug side effects from the patient’s perspective. Why was it that patients were reporting such a long list of devastating side effects while evidence in medical literature was largely absent? Were these patient experiences simply anomalies that we happened to be seeing, or was there something real going on? Without more quantitative data, these questions could not be answered.
To explore these questions, I designed several large studies, launched them online, and began collecting data, hoping that somehow the money would come in to fund the data analysis. It didn’t. And so these studies remained online, month after month, year after year, collecting data; data that needed to be analyzed and made public.
Earlier this year, I was fortunate to garner a grant for a new online project involving birth control and blood clots. The woman responsible for the grant understood the need to get the data from these legacy studies out to the public. The grant afforded me, not only the assistance of another researcher and a writer, but a much needed statistician. Per her wishes, the statistician could begin tackling the data analysis for these legacy studies, when not needed for the birth control project, e.g. during the periods of data collection. We are so very grateful that she recognized the importance of these projects.
A Note about the Data Sets
The surveys I designed were comprehensive, the data sets are massive and because they were conducted using survey software not designed for such large projects, the data sets are messy and require a tremendous amount of preparation to do even the most basic statistics. Notwithstanding the help of a part-time statistician, it will take us some months to ferret through these data sets. Nevertheless, we will get the data out. Again, if you’d like to help expedite this process, funding for a full-time statistician or even multiple statisticians would be most welcomed.
Beginning with Lupron
First in line, is one of my least favorite drugs used in women’s healthcare: Lupron. For those new to our blog, we’ve written a lot about Lupron over the years. Lupron or Leuprolide is a GnRH agonist prescribed for endometriosis, uterine fibroids, cysts, undiagnosed pelvic pain, precocious puberty, during infertility treatments, and to treat some cancers. I am not a big fan of this drug. If you have read the personal stories of the devastation caused by Lupron, or the research showing the mechanisms by which it induces damage, I doubt you would be either. Despite the decades of anecdotal evidence of serious side effects and the bevy of lawsuits filed and/or settled there is very little quantitative research delineating the scope and severity of these side effects. Given that Lupron chemically castrates its recipients, diminishing gonadal hormone production entirely, we might expect a little more research and certainly more caution in prescribing this drug. This doesn’t appear to be the case, as tens of thousands of women, men, and even children are prescribed this drug every year and have been for decades. Perhaps this is because Lupron is profitable, very profitable. In 2015, Lupron netted its manufacturers over $800 million in revenue.
What I find striking about Lupron, is not that are very few studies to support its safety and efficacy, or even that its manufacturers have been embroiled in lawsuits for decades all the while maintaining its safety and efficacy: that is common practice in the pharmaceutical industry. What is striking about Lupron is that it is a drug that effectively shuts down gonadal steroidogenesis, a key component of human health, and only a few in the medical industry think this is problematic. Here is a drug that could be used to induce chemical castration in pedophiles and rapists, if that were considered ethical or safe (and it’s not), but is used in tens of thousands of women, year in and year out, under the auspices of an effective treatment, and sometimes, even as a diagnostic for endometriosis. Worse yet, it is used on children in cases of precocious puberty, and to spur growth; two completely contraindicated uses.
How is that a drug that blocks hormones so completely, hormones that have receptors and therefore regulatory roles in every tissue and organ of the body (brain, nervous system, heart, GI system, fat cells, immune cells, muscle, pancreas, gallbladder, liver ) be considered safe? 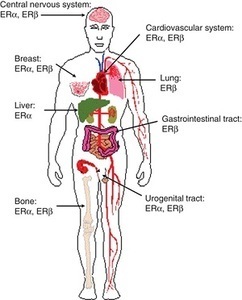 Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.
Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.
All snark aside, results from this project, and from our others studies, are critical to an emerging discussion about medication safety. Patient experiences tell us a great deal about drug safety and efficacy, if we ask. I think it’s high time that we begin asking.
Study Design
The Lupron Side Effects Survey was designed to assess potential side effects across all organ systems. Hormones have receptors everywhere: it stands to reason then, if we deplete those hormones rapidly and continuously, there will be effects wherever those hormones play regulatory or modulatory roles. Of course, since estradiol, the primary hormone affected by Lupron, is critical to mitochondrial morphology, and thus mitochondrial energetics, anywhere there are high demands for energy, the nervous system, the heart, GI, musculature, we might anticipate a high degree of effects in those systems as well, especially with longer term use and as the damage accrues.
What we didn’t know, and won’t until we fully analyze the data (what is presented here is only the beginning), is in which systems the side effects are most severe (do they follow the path of mitochondrial energetics or some other yet to be identified pattern ) and when (do they present early or late, relative to use?); which women were more likely to have side-effects (are there health characteristics that make side effects more likely or more serious?); is there a dose-response curve for side effects (do higher doses mean greater side effects – sometimes with hormones, this isn’t the case); or how the side effects cluster together (did they cluster by organ or tissue system or by some other variable, like energy demands?). Most importantly, we didn’t know whether Lupron was clinically effective at reducing the symptoms for which it was prescribed. There is some evidence to suggest that while pain symptoms associated with endometriosis may show a statistically significant reduction, particularly while the woman is taking the drug, the reduction was neither clinically meaningful nor long lasting. That is, symptoms may diminish by a few points on a pain scale while on the drug, but not abate completely, and then inevitably return upon cessation. In light of the potential side effects induced by this medication, one would expect nothing less than a large clinical reduction, even remediation of the disease process itself, as the only fair trade off. It is not clear whether Lupron can provide those benefits. None of these questions have been answered in the medical literature, despite the use of this drug for many decades.
Lupron Side Effect Survey Basics
The study was launched in 2013. The goal was to get 500 respondents, evaluate, redesign and relaunch follow-up studies. We reached the 500 respondents within a few months, but absent funding, were not able to perform the analyses. So I left the study up to collect data passively (no longer advertising it), until recently.
When we closed the study, we had over 1400 partially completed surveys. For robustness, we analyzed only those surveys that were over 90% complete. That netted data from over 1000 respondents (the number of respondents for each question varies and is listed below with each item). The survey was anonymous, voluntary, and included informed consent.
Survey respondents were asked to provide basic demographic information, answer questions about pre-existing conditions, reasons for Lupron prescription, Lupron dosage, and degree of efficacy pre, during, and post Lupron usage. To capture the range and severity of potential side effects, survey respondents were asked to indicate the presence/absence and severity of symptoms experienced relative to their Lupron usage with a 0-4 Likert-type scale (0=None, 1=Mild, 2=Moderate, 3=Severe and 4=Life threatening). And yes, we recognize that ‘life-threatening’ is not an appropriate indicator for some types of symptoms. For consistency, however, we used the same rating scale across symptoms. One hundred and eighty possible symptoms were assessed.
This post will review range and severity of Lupron side effects. Subsequent posts will address efficacy, side-effect clustering, patient characteristics predicting side effects, side-effect dose-response curves and other topics.
Demographics
Survey respondents (n=1064) were largely Caucasian – 86.6% (African American -4.7%, Hispanic -2.6%, Other – 2.3%, Asian – 2%, American Indian/Alaska Native 1.6%) and educated (30% – some college, 34% – BA/BS, 15% – MA/MS). The average age of the survey respondent was 35.36 (SD – 8.63), while the average age at which Lupron was prescribed was 29.9 (SD – 8.2). Among these respondents, Lupron was most commonly prescribed for endometriosis (88%), painful periods (33.5%), heavy bleeding (26%), ovarian cysts (18%), PCOS (4%), IVF (4%), anemia (3.9%), breast cancer (1%), ovarian cancer (.4%), precocious puberty (.2%), other (8%). Respondents could select multiple answers.
For the discussion that follows, see the interactive graphic below. We will be discussing symptom categories from left to right. The categories of side effects are grouped, to some extent, by system involved or by symptom characteristics. To view the side effects, click any of the boxes below. The side effects within that category will appear, along with the number of respondents who answered that question. Click again on a particular side effect and the severity of the side effect is displayed by percentage of women who experienced each severity level. Click in the white space within the graphs to move up a level (note, this is a little tricky in the categories with lots of symptoms). The size of the graphic does not display well on mobile phones and/or when using the internet browser Internet Explorer. For the best viewing, please use a computer screen.
Patient Reported Side Effects Associated With Lupron
General Side Effects and Allergic Reactions
Compared to the frequency and severity of other symptoms experienced in association with Lupron, side effects relative to the injection itself and those that would be characterized as allergic reactions, itching, swelling, etc., were uncommon in most of the respondents, except for injection site pain, which was experienced in varying degrees of severity by over 70% of the respondents.
Sex and Libido
As one might expect with medication that chemically castrates its users, reductions in libido and other symptoms whose net result diminishes sexual interest and ability were common. Some degree of a loss of interest in sex was experienced by all but 23% of the women, with 38% reporting a severe diminishment in sexual interest. Nearly 44% of respondents reported moderate to severe pain during sex which may explained to some degree by the almost equal percentage of women reporting moderate to severe vaginal dryness. Other symptoms reported included breast pain, swelling, and to a much lesser extent, discharge.
Muscle and Joint Pain
Up to 50% of the women reported moderate to severe muscle and/or joint pain. This is notable inasmuch as for the majority of the women prescribed Lupron, pelvic and abdominal pain associated with endometriosis is the driving factor for the use of this drug. It appears that we may be trading pain in one region of the body for another.
Gastrointestinal and Related Symptoms
Here again we see that a large percentage of women (from 15-50% depending upon the symptom) report moderate to severe gastrointestinal disturbances from nausea, vomiting and diarrhea through constipation and even bowel obstruction. Moderate to severe bladder pain was common (~31%) as was difficulty in urination (~19%) and bladder control (~18%). Since bladder pain and interstitial cystitis are co-morbid with endometriosis, it is difficult to determine if these symptoms were precipitated or exacerbated by the Lupron or simply associated with the endometriosis and thus, not remediated by the medication. We will attempt to disentangle those relationships with further data analysis and in subsequent studies.
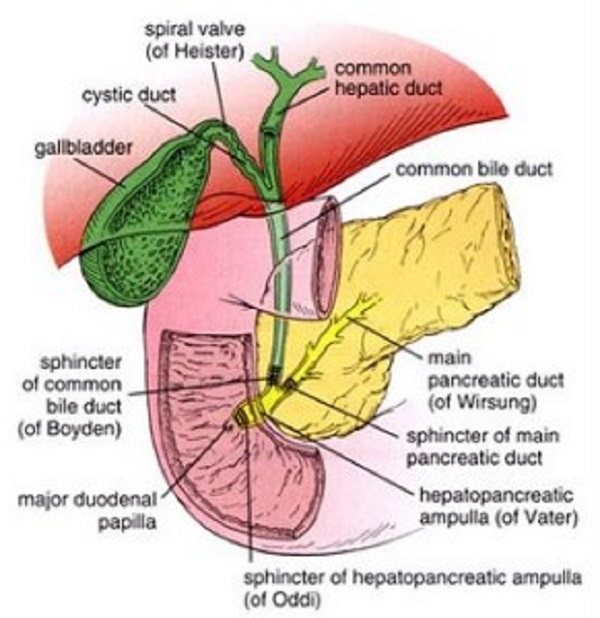
Of note, gallbladder disease (~6.2% – all categories combined), gallstones (~3%), kidney disease (2%), kidney stones (4.5%) and renal failure affect a smaller but noticeable number of Lupron recipients. This consistent with adverse event reporting elsewhere. Similarly, non-alcoholic fatty liver was noted in ~6.6% of the survey respondents.
Bone, Skin, and Related Symptoms
Bone formation is particularly hard hit by the diminishment of estradiol. Bone related symptoms are some of the most commonly reported side effects ascribed to Lupron. Research suggests Lupron induces a 5-6% decline in bone mineral density over just 6-12 months of use. Read more on the mechanisms by which Lupron induces bone loss.
Almost 20% of the women who completed the survey reported some degree of osteoporosis, and 16% reported cracking or brittle bones, 42% reported toothaches (9% severe) and 26% had cracking teeth. Osteonecrosis was reported by 3% of the respondents. Skin and hair symptoms were common and affected a sizable percentage of the respondents as well. What we failed to ask about were fractures in the spine and pelvis or osteoporosis in the jaw; side effects that commonly appear in post Lupron discussion boards. We will do so in subsequent surveys.
Temperature Dysregulation
As expected by a drug that induces a rapid menopausal state, vasomotor symptoms with temperature dysregulation were prominent afflicting ~90% of the respondents. Severe hot flashes and night sweats were reported by over half of the study population.
Metabolic Symptoms
Estradiol affects insulin regulation and general metabolism, so it stands to reason that if concentrations are diminished significantly, metabolic disruption would ensue. Hypoglycemia was reported by about 15% of the women, while hyperglycemia was reported by about 6%. Similarly, increased hunger and thirst were prominent at least 50% of the population, along with rapid weight gain (mild 19.2%, severe 25.9%). In contrast, rapid weight loss was reported by 12% of the respondents. New onset diabetes, Type 1 and Type 2 was reported by ~1% and 2.8% respectively. As we perform more advanced analyses, we will try to more fully characterize the metabolic changes in different groups of women.
Cardiovascular and Respiratory Symptoms
We know that the estrogens and androgens affect heart function via multiple mechanisms, both at the receptor level and via more global changes to mitochondrial functioning. What we don’t know is what impact blocking those hormones so abruptly and completely and sometimes even chronically, has on heart function. Clinically, the results of this survey point to dysregulated blood pressure (BP – 12.5%) and heart rate or rhythm (24.7%) with a trend towards the elevated measures for blood pressure (24.4% – all, 13.3% moderate to life threatening) and heart rate (27.7% – all, 22% moderate to life-threatening. However, there was a noticeable percentage of women who experienced lower blood pressure (16.4%) and heart rate (6.1%). At least 10 women experienced a heart attack, 36 women developed mitral valve prolapse, 10 women developed blood clots in the leg and 8 women had pulmonary emboli. Difficulty breathing and sleep apnea were reported by 22.2% and 15.6% respectively. As we do further analyses we’ll be able to more fully characterize the pattern of cardiovascular symptoms.
Brain and Nervous System Symptoms
The next five sections of the graphic represent the scope and severity of symptoms associated with the nervous system. Though categorized distinctly for purposes of display, the distinctions are somewhat arbitrary as the symptoms within each category represent those related to the brain and nervous system. Arguably, many of the cardiovascular symptoms discussed previously may also represent nervous system symptoms, possibly suggesting some degree of autonomic system dysregulation.
Headache, Migraine, Dizziness, and Seizures. A large percentage of women experienced headache and migraine pain, frequently rated as severe or life-threatening (27.2% and 28.3% respectively). Dizziness was common (69.4%), as was vertigo (46.9%). Sleepiness (68%) and fatigue (87.3) were common, but interestingly, also insomnia (76.4). Seizures reported by 5.1% of respondents. Falling (17.1%) and difficulty walking (27.9%), perhaps indicating balance issues, were also reported. TIAs were reported by 11 women and full strokes by 3 women. (Nervous System Symptoms).
Myoclonus and Neuropathy. Shaking, jerking, numbness, spasms and tingling were experienced to some degree by 15%-35% of the survey respondents. A sizable percentage of women reported moderate to severe symptoms. Muscle weakness was reported by 11-34% of the respondents whereas limb and/or facial paralysis was experienced 3-4% of the women. (Neuromuscular, Sensory Perception and Motor Control).
Hearing and Vision Disturbances. Some degree of blurred vision was experienced by 46.5% of the women, with a little over 20% rating the symptom moderate to severe. Partial loss of vision was reported by almost 10% of the women, half of them indicating moderate to severe loss. Similarly, almost 20% reported some hearing impairment. Similarly, hypersensitivity to light or to sound was indicated by 35% and 37.5% respectively. (Sensory and Motor Symptoms).
Speech and Language Disturbances. Fully 20-50% of the respondents reported difficulty with basic communication, everything from difficulty speaking and finding words to difficulty understanding speech, reading and writing. (Sensory and Motor Symptoms).
Mood, Memory, Mental Health and Affective Behavior. The brain is a major target of and source for steroid hormones. Estrogen receptors are co-localized on neurons and affect neurotransmission, neurite outgrowth, synaptogenesis and myelin growth and estradiol is generally considered neuroprotective. The prefrontal cortex, hippocampus, and amygdala, responsible for regulating directed behavior, memory, and emotion, have high densities of estrogen receptors. Depleting estradiol would be expected to have a significant impact on these functions, and it did. It is here that we see some of the most troubling and least well appreciated (by the medical profession) side effects associated with Lupron. A significant percentage of women reported severe psychological disturbances ranging from depression and anxiety (>50%) to suicidality (15% severe to life-threatening). Visual or auditory hallucinations were experienced by ~12%, with >6% reporting moderate severe issues. Moderate to severe frontal cortex issues like dulled or inappropriate emotions, lack of motivation, impulsiveness were reported in 25% to over 50% of respondents. Moderately to severely altered mental states (delirium, disorientation, confusion) were reported by 6%-25% of the women. Moderate to severe diminishment in memory capacity was reported by at least a third of the women. This is in addition the difficulties with language reported above. (Mood, Memory and Mental Health).
General Impressions
Consistent with the case stories and patient comments on message boards related to Lupron side effects, the majority of women feel rotten while on this drug. This is to be expected given the global distribution of estrogen receptors. The brain and nervous system seem particularly hard hit. Again, this is understandable given the density of estrogen receptors in the brain and the modulatory role it, and other steroid hormones, play in neurotransmission. By depriving the estrogen receptors of their cognate ligand, estradiol, Lupron fundamentally alters brain chemistry, abruptly and thoroughly. Perhaps even more troubling, estradiol is required for mitochondrial functioning. By depleting estradiol, the mitochondria are impaired, and with that impairment comes a long line of compensatory mechanisms that will ultimately derail not only mitochondrial capacity but also the capacity of all of the cell functions that require healthy mitochondria. The fact that we see such severe side effects attributable to nervous system function would be expected with estradiol depletion.
We Need Your Help
This post was published originally on Hormones Matter on September 1, 2016. Since then, we have lost our funding to complete this and the other ongoing studies. We have enormous data sets like this one on medication adverse reactions waiting to be analyzed and published. Without funding, however, these data will never see the light of day. If these issues are important to you, please contribute. If you know of an organization or benefactor interested in understanding short and long-term medication and vaccine reactions, please refer them to us.
Yes, I’d like to support Hormones Matter.
Photo by Diana Polekhina on Unsplash.











HI CHANDLER
I had a nightmare for 15 months from Lupron during prostate CA treatment.
15 months into it, I was limping along using CNS stimulants to compensate hideous congnitive problems , saved my life. I began to have severe muscle joint pain and neared a state of disability. I was diagnosed with polyarthroalgia rheumatica, was given predisone. Within 12 hour my pain and functional problems cleared by 70 to 80 percent. Including the 15 months of fatigue, cognitive , memory and other problems that began at the time lupro treatment began.
It may be causing autoimmune problems in the brain, and other areas of the body.
Hypothetically could something like chronic gonadotrophin, or human chronic gonadotrophin (HCG) be used as a semi antidote for the effects, if someone needed to stop Lupron rapidly without waiting months for it to finish?
What about MEN problems? is the Lupron for Womens only?
Being as Chris W asks about men i will reply.
We are treated pretty much like you ladies on here,with much the same side effects apart from the obvious differences,i do not know if Ms Marr would agree on that.
I am fully 2years clear of my last jab,but my side effects have certainly not gone,so all this talk of them clearing up after time is absolute rubbish.
I will admit to anxiety before the jab but now it is way higher and i am sure that once the lupron injections are over [i had 18 months] apart from psa checks little more is done.I feel like we are left to deal with everything else by ourselves,i do not know if other people on here feel this way?My own thoughts on this are like it says on here you simply cannot play with our hormones this way and not expect trouble,it is akin to putting diesel in a petrol car,it will not run.
My oncologist said it would keep me alive but he did not say what kind of a life it would be?
Yes life is precious and my lovely wife is glad to have me,but i am not who i was i am fat around the middle with boobs up top.No sexual feelings since the very first shot and i do not think i will ever have them again,i ache all over,and have to beware of diabetes and cholesterol levels.I tire very easily and get strange tingling feelings in my shoulder and neck that only began a few months ago,can new effects spring up so long after ending lupron?
May i say thank you to sites like this because otherwise i would not have known lupron could do so much to our bodies and mind, it seems you have to find out for yourself no one tells you.
For some lucky people it does work with little problem and good luck to them,but for others it can be a completely different story
Garry, since we do not have any Lupron stories from men, would you be interested in writing up your case history/story and allowing us to post it on HM as an article?
Thank you so much for your reply Ms Marrs,sorry for missing the[s]from your name.I will do my best to give a review from a male perspective for HM.
I do live in England so it will be from a British point of view not American.
That would be great. Use the contact form to send me a note when it is ready and I will send you my email address from there.
https://www.hormonesmatter.com/contact/
Four months after my sub-total hysterectomy in December 2014 I was still having the same pelvic pain symptoms. My gynecologist didn’t know what else to do other than to use Lupron for 3-6 months to see if it would diminish my pelvic pain; if it did she said the ovaries would have to come out. She told me she was using it as a diagnostic tool and if I didn’t try it she “would drop me as a patient.” More accurately, she screamed at me, started frantically waving her hands above her head and hit me with her pen. There were times I wish I had a witness to some of the behaviour I was subjected to over the years; this was definitely one of them. I took the prescription home but didn’t fill it. I was not only shocked by her behaviour but also a little leery about being souped-up on yet another Rx with horrible side effects.
I held off until Sept 2015 when I decided I couldn’t stand the pain anymore. My first injection was in October and I seemed to handle it quite well. I had relief from my pelvic pain within two days and a bit of mild dizziness that went away after about a week. The reduction in pain allowed me to go out for walks 2-3 times per day, which is something I hadn’t experienced for quite a long time—it was great to be walking again. Then I started noticing some strange symptoms every two weeks after the injection.
The first time it happened the symptoms were so mild I brushed them off as a minor cold bug: body aches and pains, sniffles, lungs slightly congested, watery eyes, my hearing was off and my eardrums felt plugged up. I thought maybe my daughter brought a cold bug home from school, but these same symptoms happened exactly two weeks after the Lupron injection and every time the symptoms kept getting stronger. When I was due for my 4th injection I knew something wasn’t right. My regular gynecologist wasn’t in and I’m glad she wasn’t. The one I did speak to about my symptoms told me to not take it anymore. He looked up my symptoms in a large pharmaceutical reference book; Lupron was listed as having “flu-like symptoms” in its trial phase but had no further information. I was told to go home and just let the effects “wear off.”
Between December 2015 to February 2016 I had 11 visits to the ER for worsening flu-like symptoms: strong body aches and pains that felt like I had been hit by a train, congested lungs, coughing up greenish-yellow fluid and the same gross mucous was coming out of my eyes and ears—my lungs were so congested I was gasping for air—I was terrified! They tested for bacteria, throat and nasal swabs, full blood work—everything came back negative and it wasn’t pneumonia. I didn’t even have a fever. The last ER doctor I saw actually called ABBVIE to see what to do. He told me they are supposed to have something like a WHIMS on all their products in case of adverse events. Well, guess what? They didn’t! The ABBVIE representative told him they knew about the severe flu-like symptoms in their trials with Lupron but they did not follow those patients to record their outcomes—in other words there was no due diligence before releasing their product to the public. They don’t even know if those patients are still alive. I was given an IV to prevent dehydration and placed on oxygen until my vitals improved; even then I was sent home without any concrete advice on how to deal with the side effects other than “it should wear off” and “if it gets worse don’t hesitate to come back”—like now isn’t worse. I asked the ER doctor if he is filing an adverse event report to Health Canada or the FDA, he said that is for the patients to do but in your case, I wouldn’t worry about that, we don’t know if that is what is causing your symptoms, it could just be a viral thing. I was about ready to flip my lid! He told me earlier if it was viral I would have a fever because that is what your body does to fight off infection and viral infection symptoms build up, peak, and then you start feeling better—these symptoms only occurred two weeks after each and every injection. I felt like I was talking to a brick wall. Do you know it took another 4 months for that damn Lupron to wear off? The entire time I was scared shitless because I was gasping for air while this green mucous is pouring out of my ears, eyes and lungs. I would panic, cry, and then have to calm myself down because crying would congest my lungs making it harder to breathe. I have never been so scared in all my life.
I did go back to the gynaecologist that prescribed it and she had the nerve to tell me it’s not her problem and to go see my GP. My GP told me since she didn’t prescribe it that it’s the gyn’s problem; went back to the gyn to tell her what my GP said and she threw another hissy fit because apparently, I wasn’t on it long enough to satisfy her 6-month requirement. My husband didn’t believe what I was telling him so I got him to call the office to rebook an appointment so we both could talk to her. At this next appointment she placated my husband and refused to look me in the eye while she was speaking. I reminder her of everything she said previously: that it is her problem because she is the prescribing doctor, that my pelvic pain symptoms did improve while on the Lupron, that my adverse effects were directly related to the drug as my worsening symptoms occurred exactly two weeks after each and every injection, I was tested at the ER—it was not viral or bacterial and the ER doctor called ABBVIE and they had severe flu-like symptoms listed during their drug trials but not followed up. I informed her I filed complaints with both Health Canada and the FDA. She got up to check on my ER visit reports, while she was gone even my husband noticed she wasn’t talking directly to me, only to him and that I did meet her requirements—Lupron for at least 3 months, if the pain is relieved then it means the ovaries need to come out. My husband was ready to have it out with her when she came back. She kept trying to placate us, saying things like “I don’t know what to do”. I kept pushing for an answer—what was causing my pelvic pain if Lupron was the diagnostic tool—what was she using it to diagnose? She never mentioned “Endometriosis”. I asked her if it could be cancer–no answer. I finally said, “If you don’t know what to do then send me to someone who has more experience dealing with complex gynecological issues. I want a referral to the Women’s Health Sciences Centre in Halifax.” I hate to think of what would have happened if my husband wasn’t there to keep me centered; even he was getting frustrated by this gyn. She finally agreed to send a referral to Halifax. As we were leaving, she told my husband she was retiring in a couple months so do not bother contacting her for any further concerns. I found out just a few days ago she is still working as a gyn—so she basically lied to my husband. What a piece of work! I don’t understand how doctors can behave like this. There has got to be some kind of benefit, either monetary kickbacks or endorsements, to blindly stand behind a drug like this and totally ignore what the patient is telling you to your face.
Lupron needs to be discontinued. If these drug companies can’t do a long term followup on patients during the drug trials and issue WHIMS style information on ALL adverse side effects, it should not be used on the general population. I only found out recently it has caused 1500 deaths worldwide and there’s an entire website dedicated to the ongoing lawsuits from this drug.
Do you know who has the on going Lawsuit? And, Where did you find out about the 1500 deaths? Do the symptoms ever where off?
My wife is suffering with extreme muscle and joint pain. I don’t know what to do to help.
Thank you for studying this drug. I’m transgender and started monthly Lupron injections in November 2018, to suppress testosterone levels. My last injection was in July 2019. I skipped the August injection due to these symptoms: extreme thirst (I need to drink over a gallon of water a day, even if I’m just sitting around the house); extreme thirst at night, awakening with dry lips, mouth and tongue, even though my bladder is full); increased bowel movement frequency (6-8 a day); constipation if my hydration levels fall; difficulty falling asleep; frequent night time awakenings due to need to urinate, coupled with difficulty falling back to sleep; greatly decreased ability to digest fats; queasiness and headache from even one alcoholic beverage; and hair loss, extreme scalp dryness, and raised rashes on my scalp. By the way, diabetes has been ruled out by my doctor and Endocrinologist. Unfortunately, the other 2 T blockers typically used by TFs also caused me problems, which was why I started on Lupron to begin with. It is strange that the manufacturer and other formal medical web sites show these symptoms as being very rare. I wasn’t too concerned about starting on this drug as a result of the information from those sources. As my symptoms increased in severity, and as they’ve continued now 7 weeks after my last injection, someone told me about your site. I’m astounded and saddened that your survey unfortunately shows a much higher incidence of severe side effects from the actual users of Lupron, and my heart goes out to those so afflicted. Needless to say, no more injections for me, and I hope my health, and the health of others who are or were on this drug, has not been permanently impaired.
Hi! I’m so glad I stumbled upon this website! I’m 52 years old. Ever since 8th grade I’ve had excruciating cramps and heavy bleeding. The only time I didn’t have pain was when I was pregnant. I went to 9 different gynecologists before finding one who could make the pain go away. I was too young for a hysterectomy so Lupron would put me in temporary menopause. I wasn’t having any major side effects so I stayed on Lupron for 19 months before my hysterectomy. I was then diagnosed with adenomyosis. I had horrible stomach issues and underwent all kinds of expensive tests & scans. I had an ultrasound done & a gallbladder scan. I now also suffer from many other issues…joint pain, bone pain, exhaustion, insomnia, forgetfulness, vision & hearing issues, occasional speech issues,migraines, anxiety, depression. I take a lot of prescription medication for all of these things. I’m shocked that I’m just now discovering a link to Lupron! I thought it was just me. I had no idea it could be side effects from the Lupron. I feel like there’s always something wrong with me. If I had known there would be long term side effects, I would have opted to do the hysterectomy immediately. Here I am 15 years later and now my daughter is presenting with the same gyno issues. Ugh. NO LUPRON FOR HER!!!!!
Dear Chandler,
I must say, I have great respect for you and appreciate the information you are putting in front of everyone.
I am a male who was prescribed Lupron at a young age with goal of growing taller (although I did not have a hormone deficiency) while also taking HGH. I have recently been able to tie a list of health issues I am dealing with back to the drug (Lupron). Hip pain, back/neck pain, sexual issues, blurred vision, chest pain, etc. My biggest struggle has been finding doctors who can help. While some doctors call me crazy as minimal side effects are illustrated in medical literature, others simply have no knowledge of how to help. I have reached out to the doctor who prescribed the mediation and she denies any of my issues relate to Lupron. Is there anybody you may be able to put me into contact with to help prevent things from getting worse (they have been year over year). I live in Los Angeles. Thank you again for all your efforts.
Thank you for your work. My daughter started on Lupron at 7 years old, a year ago. She has had 4 shots thus far and is currently month overdue on her 5th. Due to some recent health issues I started researching in depth the actual side effects, short and long term of this drug and consequently decided to stop allowing it. The thought that I have sentenced her to a lifetime of health issues weighs heavily on me. Now I am looking to see if there is anything I can do to prevent further damage at this point. Is there any research you can point me to that can provide me with any information on repairing mitochondria and possibly stopping the cascade effect? Are there any other actions/treatments we can inact that you feel may possibly help her at this point to prevent or minimize future health problems?
The only way to prevent long term consequences, is from here on out to heal and protect her mitochondria. We have lots of articles on this and I wrote a book on it, but the gist is an absolutely clean diet, organic, no junk food, avoid as a many toxicants as possible, including unneeded medications/vaccines, and she likely need to supplement with a variety of nutrients that the mitochondria is absolutely dependent upon. If you can keep the mitochondria functioning, then they will repair the damage done. Since they regenerate, over time she’ll have more healthy to unhealthy mitochondria. For additional information on mitochondrial, read the articles, the book, and considering joining the Facebook group – Understanding Mitochondrial Nutrients.
I cannot find this FB group and would really like to join. Can you please post the FB link?
Which FB group?
I just finished my 6 injection in the end of January. I have had a horrible experience on the 1/mo Lupron 3.75 injection. My doctor did a hysterectomy in August 2017 due to fibroids and cysts. Ultimately, that was my decision as I knew they would return and we were done having children. When they performed my surgery, it was discovered that I had endometriosis. My doctor suggested the Lupron to keep it at bay, and to allow me to keep my ovaries for a while yet. About 4 months into my injections I was experiencing bone and muscle pain. My migraines were worse. Insomnia nights sweats, GI issues. I’ve been thru the ringer testing for a GI disorder, Celiac’s, gallbladder, hernia. I’ve gone thru thousands of dollars worth of tests since January. While discussing my symptoms with my OB, she said they sounded musculoskeletal and referred me to a rheumatologist. Thankful for that. I just saw him this week and he said that the symptoms sound like Fibromyalgia, but that the Lupron side effects can mirror fibro, and this is all likely from my injections. I’m 36 yo, married, with an 8 year old son. My husband wants his wife back, and my son wants his Mom back! Regretting the choice to go with Lupron.
I was on Lupron shots for 18 months in 1999 and 2000 for endometriosis.I am now having severe health problems and am seriously thinking it is from this treatment. I just recently had an MRI of my brain and am awaiting the results. This is the best article I have read on this. I would not ever recommend someone taking this drug. I feel it has really caused me a lot of anxiety and worry that could have been prevented had my doctor known more about the adverse effects.
I am curious to know the results for your MRI. i was on lupron, later diagnosed with Multiple Sclerosis, which I do not believe I have, I believe I have lesions due to the lupron and I am trying to find some correlation.
Having a daughter now almost 13 I am facing a terrible decision. Do I proceed with lupron in the form of puberty blockers to postpone the signs of womanhood before transgendering later in adolescence or giving her low dose provera? The well meaning doctor claims there are low risks and everything is reversible but having read of all these adverse health effects I don’t know what is the safest risk. My child has dressed as a boy for nearly 2 years and is extremely distressed by her/his developing breasts and periods. Most transgender literature is very supportive of using lupron in this manner, however who knows what the long term effects will turn out to be??????
The side effects of Lupron are lifelong for many. Depo provera has its own list of side effects. These are difficult decisions. As a mom, I would search for another option. There are Facebook groups devoted to the illnesses initiated by Lupron. I would read those and have your child read those too before considering this treatment.
This might be useful. https://4thwavenow.com/2017/10/25/born-in-the-right-body-introducing-4thwavenows-new-spokesperson-mom-of-a-teen-desister/
I am not one to ever comment on these but I feel this is important. I would love to be a part of your future research. I never finished all the Lupron that my dr prescribed because it was awful. I took Lupron in 2006 or 2007 and my life has never been the same. Honestly the hot flashes, muscle and bone pain and anxiety have never gone away. Before using Lupron and finding out I had endometriosis I was a very healthy individuals. I gained over 60 pounds during the process and don’t know if I ever go a day without thinking why did I allow myself to use Lupron. I was 21 and had a dr. I thought had my back, I did question bone density issues and was told that is nothing to worry about. I wish I could know what I would feel like today had I not ever taken Lupron. It took years to get pregnant as I never ovulated consistently and then staying pregnant was a whole nother this. Anytime I heard someone mention Lupron I cringe and tell my story, but tell them to do a lot of research before.
I had Lupron injections in 2003 for Endometriosis and have steadily been experiencing different health issues since. My Dr and I have batted around several different things and go through semi regular tests to see what it could be (other than Endo ?,Psycho-sematic?)
Adding up all of the ‘odd things’ that I experience (but shouldn’t) eventually – it seems to circle back around to having had Lupron.
I took 4 shots in 2010 for endometriosis and still have joint pain and memory issues. This was very insightful. Thank you for your research.
My Dr, a neuro endocrinologist has done extensive research on epilepsy and the use of lupron plus add back hormones has suggested this treatment for me. I am 51 and have grand-mal seizures during short menstrual cycles. My periods have been erratic in flow and length for 4 years now. My FSH levels put me into the perimenapausal phase. I have failed basically all epilepsy drugs at this point. We are out of treatment options. The meds aren’t working. We tried progestin lozenges to stop my period. It didn’t work. The last remaining option is lupron + add back. By age, we would think menapause is approaching but my quality of life (migraines/seizures/cramps/moods and on and on) is poor at this point and it could be 1 month, it could be 5 years until I go through menapause. Who knows.
Do you feel the same way about lupron for someone like me, on the way to menaupase taking lupron to shut down my menstrual cycle because the erracible hormones are causing seizures? (We have been tracking it.)
Are the risks for all types of treatment with Lupron the same?
I do understand there is a risk of seizure for the first 10 days of the treatment, but I am having them anyway…. it is hard to asses risks.
Thank you for your time and insight.
The damage Lupron causes is the same for everyone inasmuch as the mechanisms of action of this drug do not vary from person to person. They are what they are. Lupron damages the mitochondria in some fairly significant ways, particularly because it depletes endogenous estradiol. https://www.hormonesmatter.com/lupron-estradiol-mitochondria-adverse-reactions/
Whether and to what degree anyone taking the lupron experiences the side effects clinically, has a lot to do inter-individual and even intra-individual genetic/epigenetic variability and the body’s ability to withstand the stressor/damage – e.g. does it have the metabolic resources to overcome the damage and compensate while the damage is accruing. It also has to do with dose and duration of use. Essentially, it’s a threshold effect. The drug does the damage, the question is whether or not the individual can withstand it.
Since you have been on a lot medications, most medications damage the mitochondria, and you already have seizures, your mitochondria are probably pretty bad already.
The idea that add back therapy would help, particularly synthetic hormones, which though molecularly similar, they are not identical, is ludicrous. They metabolize differently, into different compounds which the body doesn’t know what to do with. Worse, they deplete endogenous hormones and their metabolites which are actually needed for a lot different functions. To boot, synthetics further damage mitochondria.
Where in the cycle are your seizures? Have your hormones been measured during these periods of high seizure frequency? Similarly, what is your diet? Sugar intake? Ketogenesis works for a lot of folks with seizures – proteins/fats no sugars. What is your salt balance? Interestingly enough, too little salt induces kindling and seizures. Salt deficiency is a huge problem that few recognized because of all the marketing for low salt this and that. There are a lot of options, non pharmaceutical, that could provide you relief without the damaging effects of Lupron. I am not a physician, so this cannot be construed as medical advice, but it is advice to dig deeper, do more research and consider fully the options. I would also invite you to share your health story on the blog as a post so that other patients, researchers, and physicians can see it and offer insights. There is likely someone out there who has a solution, but you have to become your expert to some extent.
Thanks for your reply. I haven’t had my hormones measured during a seizure. The seizures come without warning and are grand mail so it would be hard to measure hormones during them, per se.
The add-back would be bioidentical hormones and the seizures come a few days after my period ends, on cycles that are less than 25 days. I have had had 6 seizures on short cycles. My dr tells me that his published research shows that women whose cycles are less than 25 days or more than 40 days are at greater risk of seizure and are tied to estrogen spikes in the cycle and anovulatory cycles. The lupron shot would be given on day 1-10 of the cycle once a month. It would cause my period to stop. He has a 75 percent success rate at stopping the seizures. My neuroendorcrinologist has 3-4 decades of research and is very well respected. My regular epilepsy specialist says he helps many women that no one else can help. Yet I am afraid.
Unfortunately there are no actually NO other treatment options for me at this point–I have exhausted all standard medical options for the type of seizures I have. I am left with Lupron with add back or Ketogenic/or Modified Atkins– my ideas –I asked him about it. both are very difficult to follow but are shown to stop seizures. he says meds won’t work for me at this point. The spikes in hormones will override them.
Herbs, are not safe for people with epilepsy (no research on how they interact with the meds so they could lower the seizure threshold).
As for my diet, I have been following the Always Hungry! eating plan for about a year. It’s higher protein, higher fat and complex carbs. The only sugar I eat is fruit and salt intake is pretty normal. I don’t drink at all. I had gained “that typical 10lbs in perimenapause,” but I have since lost it. My weight is normal now. I am pretty slim.
I will take your advice and post on the blog…appreciate your time. I am not ready to do anything at this point. But I am suffering and looking for relief from the seizures and perimenapause. Seizures take months and months to recover from (not typical) and the hormones spikes from perimenapause are pretty much ruining my life. Gynocologist says whatever neuro.endocrynologist says….he’s kind of the “guy”
I am frustrated. PS can’t take unapposed estrogen like many women take during perimenapause. That can cause seizures too….
My daughter had a Lupron infusion when she was ten years old for precious puberty. Now she has full body Reflex Sympathetic Dystrophy at age seventeen. It is horrible.
I am afraid that is not uncommon. It is likely do to mitochondrial damage. You might consider reading up on mitochondrial damage and lupron and other medications and how to support the mitochondria in their functioning. We have a number of articles on this topic on this blog and will have a book coming out on mitochondria, and specifically, the role thiamine in mitochondria later this spring. There are several RSD cases covered in the book.
I am in the process of deciding how to treat my 7 year olds CPP. I have read enough about Lupron to know that it is not safe. Is Supprelin the same thing? Do you have any research as to a better alternative for Lupron?
Yes, it works by the same mechanism.
Have you normalized the data for the occurrence of these side affects in the general population?
I took 3 months of Lupron and had terrible anxiety that lasted for months after the treatment (but I had the anxiety before the Lupron). My doctors suggested 3 more months but I opted not to continue treatment. I have an adenomyosis and was not offered any other choices to try to have a child. I researched fMRI surgery but it is not FDA approved. I saw one of the few doctors in the country that worked in fMRI trials for treating fibroids and he said for what I had it would not be cost effective.
I had some mild side effects and I hope I will not have any lasting affects. So, I was hoping that you might have some comparisons of the occurrence of these side effect events in the normal population. Also, would the side effects reported here apply to any amount/dosage taken or is there a threshold? I would love to contribute to you data if you can send me some information. Thank you for your work!
There’s really no way to tell to what degree these symptoms would occur in the normal population because there is no such thing as a normal population that is completely unmedicated at this point. All medications to some degree or another elicit these types of symptoms. It’s just a matter of how severely. Having said that, at the molecular level, Lupron does serious damage because it completely depletes ovarian (and testicular) steroidogenesis. It is akin to chemical castration, whether given to females or males. Steroids affect every organ, tissue, cell in the body. The brain, the heart, in particular are dense with estrogen receptors. Depleting those receptors of their hormone induces all sorts of compensatory cascades. In the brain, we get all the traditional signs of psychiatric and cognitive disturbances. In the heart, rate, rhythm, BP disturbances among other things. Importantly, hormones, particularly estradiol, modulate mitochondrial integrity. The mitochondria provide cellular energy, control steroidogenesis, cell life/death cycles, stress response, among other things and so disturbances in mitochondrial integrity have wide reaching effects for all organs tissues that are highly energy dependent, the brain, heart, GI tract, musculature but also all immune/inflammatory function. Lupron effectively shuts down mitochondrial function. I have written several articles on that. Here is one. https://www.hormonesmatter.com/lupron-estradiol-mitochondria-adverse-reactions/. Unfortunately, we lost our funding and so it is not clear when we will be able to resume this project. We have a lot of data analysis yet to do and I would like to re-release an updated version based upon what we learned so far. That requires funding, however.
Hi Nikki, I too recently got the 3month injection and though I suffered from some anxiety before the drug, it has since become debilitating. I find it so hard to explain in words but when you would get anxious on the drug would you feel a sinking feeling in your heart/chest and get suddenly very suicidal and feel a strong sense of hopelessness? This is what has happened to me since getting the injection. What’s more, I have severe hot flashes every single time I have any kind of panic attack or feel even the slightest bit of excitement. I lose motivation very easily because i am also struggling to sleep, often waking up in a panic several times every night from that heart/chest feeling and the hot flashes that follow. I went to see my OB-Gyn and she prescribed some anti-anxiety meds which have done very little to help do anything more than sedate me. I have also been taking menopause supplements and calcium which haven’t helped much either. My blood pressure is sitting right on the border and i’m only 29. It’s now a month post what should have been the end of Lupron’s work in my body and I still feel like I’m in hell.
My husband is on lupron every 4 months plus Xgeva and bicaluarmite. He is starting to have pain with kidneys and bladder. Your research is very valuable because these doctors and their practices are a joke these days.
thank you for doing all you do. my daughter is 7 years old, diagnosed with precocious puberty. She’s also affected by tuberous sclerosis complex, epilepsy, autism, and delayed. She’s gained 15 lbs since September being on the supprelin implant. it’s all in her mid-section though. She was gaining rapidly beforehand (25 lbs in 11 months), but it’s more rapid now. It’s uncontrollable. After reading the survey results and many people’s own experience, my wife and I are thinking of having the implant removed. Talking to the doctor today. Thank you again
I want to echo Lynne Millican’s sentiments above. Can’t tell you how much I appreciate your wonderful work on Lupron (as well as Lynne’s). Thank you very much!! I’m 25 years post-Lupron and struggle constantly with its devastating aftermath.
My 10 year old daughter was diagnosed with Type 1 diabetes in August, 2016, after being prescribed Lupron shots for precocious puberty. She had the monthly injections for a period of eight months. Two months later, she was hospitalized in critical condition after suffering diabetic ketoacidocis. She was in a coma for two days. Not one person on either her maternal or paternal sides of the family have ever had this disease. The more I research, the more I find a correlation between her diagnosis and the Lupron injections. I was never informed of this risk by her endocrinologist, who happens to be the same doctor who is now treating her for the diabetes. I am seriously looking for another doctor and searching my daughter’s legal options.
Chandler,
This is STELLAR work – absolutely stellar. Thank you so much for all your time, effort, and determination – especially despite the lack of funding.
Because of illnesses, I’m seeing this data a bit belated, but have spent some time going thru the various categories – and the numbers are very interesting. And with more time and review, I would like to comment further.
Could I suggest a way to garner a little funds for part 2? It would be very helpful to many, I’m sure, to be able to purchase a pamphlet from HormonesMatter delineating all the data in your various categories. I’ve made a spread-sheet of sorts for myself, but a ‘copy’ from you would be best. Just a thought for a way to get some small funds to off-set a little of Part 2’s expense.
And wouldn’t it be an interesting endeavor to compile a list of the many endo/gyn studies involving the use of lupron that lack mention of adverse events – but which HAVE been *amply* funded. Imo, that would speak volumes. (And at a later time, I’d like to add my $.02 here as well.)
Thank you again for your persistence in addressing Lupron’s adverse events – it is greatly appreciated.
Thanks Lynne.