As a health writer, I must ask if adequate vitamin D can prevent and/or treat the progressive brain disease called Alzheimer’s. No one should have to endure Alzheimer’s disease (AD), a deadly cognitive disorder that the Alzheimer’s Association® claims cannot be prevented or cured.
Staggering Statistics
The number of Alzheimer’s patients is growing at an alarming rate. Nearly 44 million people worldwide have developed AD, according to Alzheimer’s Disease International. Moreover, incidences of the deadly disease are expected to increase significantly over the next decade.
About 5.3 million Americans have AD. In fact, at least three persons living in the United States will develop AD before you finish reading this brief article. Yes, every 67 seconds another American succumbs to Alzheimer’s, the most common form of dementia. (1)
The medical community’s views about why the prevalence of AD is rising at a staggering rate remain varied. Many believe genetics and environmental pollutants may serve as risk factors. Some believe the predominance of vitamin D deficiency may be linked to the mounting incidences of AD. In fact, scientific research indicates that the majority of Alzheimer patients have low levels of vitamin D.
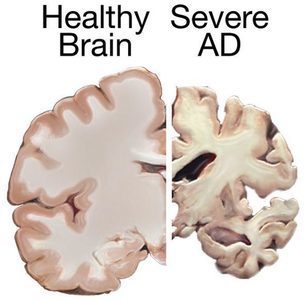
But first, let’s understand what happens to the brain when Alzheimer’s strikes it.
The Brain on Alzheimer’s
The sheer complexity of the human brain is daunting. A healthy adult brain contains approximately 100 billion nerve cells, called neurons, which connect at more than 100 trillion points in the central nervous system.
The adverse effects of Alzheimer’s on the brain are obvious to medical personnel interpreting the images. First, the brain of an AD patient is smaller than one of a healthy adult. The decreased brain size is a result of the brain tissue containing significantly fewer neurons. Second, abnormal clusters of amyloid-beta protein fragments, called plaques, collect between nerve cells in the brain. Thirdly, dead or dying neurons, called tangles, are visibly present in the brain of an AD patient.
Signals traveling through the brain’s extensive neural network form the basis of memories, thoughts, and feelings. When plaques and tangles develop in the brain, the signaling essential to cognitive function becomes disrupted. Moreover, the brain cells are destroyed, resulting in progressive cognitive issues including memory loss, poor decision-making and behavioral problems.
Vitamin D’s Beneficial Effects on the Brain
Vitamin D crosses the blood-brain barrier. And every one of the 100 billion or so neurons in the brain includes a vitamin D receptor (VDR) that influences cognitive health.
In order to regulate specific brain functions, the VDR in these cells must be turned on by receiving activated vitamin D. Without sufficient vitamin D to activate its receptors, the neurons cannot work properly.
Activated vitamin D affects the development of neurons as well as their maintenance and survival, by regulating the synthesis of nerve growth factor.
Remember those plaques and tangles that disrupt the brain’s intricate signaling system? The neuro-protective effects of this vitamin also include the modulation of signal stability within the brain’s complex neural network.
Recent Research Links Vitamin D Deficiency and Alzheimer’s
An abundance of research connects vitamin D deficiency, a condition that is highly prevalent in adults aged 65 years and above, to cognitive decline. So I explored recent research to learn more about the association.
International experts gathered at an invitational summit on “Vitamin D and Cognition in Older Adults” to provide “clear” guidance to researchers and clinicians about the role of vitamin D in Alzheimer’s. They agreed that vitamin D deficiency (a blood serum level < 30ng/mL or 75 nmol/L) increases the risk of cognitive decline and dementia in adults aged 65 and older. Their report was published in the January 2015 edition of the prestigious Journal of Internal Medicine.
Dutch researchers reviewed medical literature about vitamin D’s association with cognition in older adults. They found “emerging evidence that suggests a beneficial role for vitamin D in brain physiology.” The researchers noted associations between higher blood serum vitamin D levels and better cognitive performance. The reviewers’ findings were presented in the January 2015 issue of the journal Current Opinion of Clinical Nutrition and Metabolic Care.
Sir Michael J. Berridge, an eminent physiologist and biochemist, conducted a study at The Babraham Institute in the United Kingdom that was published in the June 1, 2015 edition of the journal Biochemical Society Transactions. His research suggests that vitamin D is the “guardian” of signaling stability. By examining vitamin D’s role in the constancy of the Ca2+ (calcium) and reactive oxygen species (ROS) signaling pathways, Berridge postulated the necessity of activated vitamin D to maintain the normal function of these critical, intracellular “cross-talk” molecules. He concluded that “a decline in vitamin D levels will lead to erosion of this signaling stability,” suggesting that a plethora of diseases linked to vitamin D deficiency are also associated with a dysregulation in both Ca2+ and ROS signaling.
Bolster Your Brain with Vitamin D
The statistics of escalating rates of Alzheimer’s suggest that your life—in some way—will most likely be impacted this deadly disease.
A breakthrough study, published June 24, 2015 in the online version of the journal Neurology, revealed that Alzheimer’s may develop 20 years before any symptoms appear. These findings suggest that we may be able to prevent this deadly disease. They also indirectly hint at the need for humans to be vitamin D-rich throughout life.
Considering the association between vitamin D deficiency and Alzheimer’s, I encourage readers to consider seriously daily supplementation with vitamin D3 and its partners, magnesium and vitamin K2.
Perhaps Michael F. Holick, MD, PhD, one of the world’s leading experts, said it best: He concluded in an article on brain health, published in a 2015 issue of the Journal of Internal Medicine by stating, “There is no downside to increasing vitamin D status for all by encouraging vitamin D supplementation and sensible sun exposure.”
Footnote 1: “Dementia” encompasses a spectrum of brain-related diseases including Alzheimer’s.
About the Author: Susan Rex Ryan, author of the award-winning vitamin D book Defend Your Life, is dedicated to vitamin D awareness. Her extensive collection of health articles can be found on Hormone Matters as well as her blog at smilinsuepubs.com. Join Sue in her “Vitamin D Wellness” FB Group to learn more about vitamin D3, magnesium, and vitamin K2 supplementation. Follow her on Twitter @vitD3sue.
Copyright © 2015 by Smilin Sue Publishing, LLC
All rights reserved.