Since we have shown that many people with complex disease patterns respond to megadose thiamine and magnesium, irrespective or their symptoms, we have concluded that disease is due to a breakdown of health from energy deficiency. We have proposed that 3 interlocking circles (as in Boolean algebra), labelled Genetics, Stress, and Energy (or Fuel) must be considered singly or collectively as the cause of any disease. Energy is the force that enables any form of mental or physical body function. Its deficiency affects one or more of the three circles.
Genetics is not often a sole cause of disease. It usually requires other factors and genetically determined disease can often be treated by epigenetic energy stimulation. Symptoms of Type 1 diabetes often appear in middle age, often after a mild stress event such as a common cold. Surely it would appear at birth if genetics was the sole cause.
Any form of stress (infection, trauma, prolonged mental stress) demands cellular energy to meet it. The hind brain controls the complex response and is automatic. This part of the brain is highly sensitive to cellular energy deficiency and thus, energy stimulation is the essential factor required to treat any disease.
Beyond Deficiency
It has been shown by Antonio Costantini’s group that mega-dose thiamine treats Parkinson’s disease, presently deemed to be incurable. They have reported similar clinical benefits in Friedreich’s ataxia (another neurodegenerative disease), Multiple Sclerosis and Fibromyalgia, suggesting that each of these diseases, rather than having separate causes, are all energy dependent manifestations of disease. Just last year, a group of researchers linked a damaged thiamine/biotin transporter gene to Huntington’s Disease. Just this month another group has found that thiamine/biotin treatment compensates for the genetic dysregulation, restores function, and rescues neuronal pathology associated with Huntington’s Disease in mice.
A publication decades ago in a prestigious medical journal reported that 252 different diseases had been treated with mega-dose thiamine, with varying degrees of success.
This information, published in peer-reviewed medical literature is startling, because thiamine, in minute doses, is thought to have its sole responsibility as a vitamin. To use it as a completely non-toxic drug offends the present model used to explain disease. Also, it demonstrates that our knowledge of vitamins is incomplete.
Children’s Health and Thiamine
While I was working at Cleveland Clinic in the seventies as a pediatrician, many emotionally disturbed children were referred to me by pediatricians in private practice in the Cleveland area. I found that the diet of these children was full of empty calories due to their indulgence with candy, soft drinks and a variety of substances usually known as “junk foods”. They had been treated with a variety of pharmacological drugs that either had no effect or even made the clinical situation worse. I treated them with large doses of thiamine and their symptoms disappeared. The explanation by my colleagues was the traditional one, “spontaneous remission”, usually used to explain a mystery cure. My explanation was that deficiency of brain energy was responsible for their symptoms. Thiamine was stimulating its cellular synthesis.
The RDA for Thiamine and High Caloric Intake
I looked up the history of the establishment of the Recommended Dietary Allowances (RDA) for these essential substances occurring in natural foods. I found that the original recommendations had been made by a committee of “experts” and there was surprisingly little science involved. There was no attempt to tie the RDA of the vitamin to the calorie concentration.
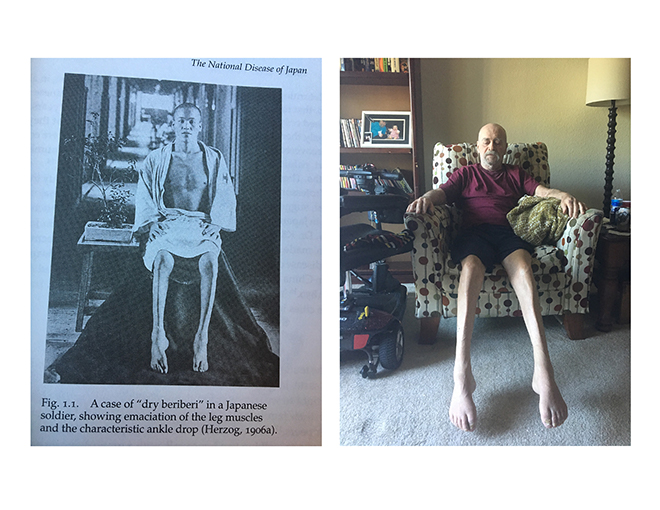
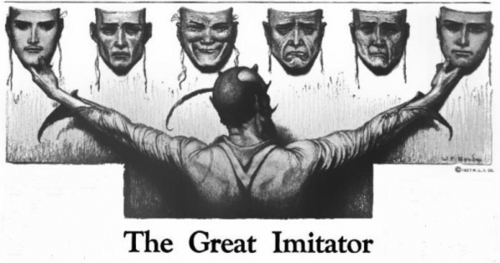
The dietary supplementation of vitamins to selected foods by the food industry was thought to have completely removed vitamin deficiency disease from America. Consequently, doctors in practice are commonly seeing patients with many symptoms and failing to recognize the ancient disease known for centuries as Beriberi. Because the laboratory tests, used to confirm the nature of the disease, are normal, the many symptoms described by the patient gives rise to a diagnosis of psychosomatic disease by the doctor. Even worse, the patient is told that “it is all in your head” and he or she is advised to “pull him (her)self together”.
Deficiency of thiamine and magnesium, both essential to cellular energy production in the body, need to be in a concentration that is sufficient to oxidize the calorie concentration. That explains why the concentration of blood thiamine is usually normal in this common polysymptomatic disease, because the doctor fails to recognize the overload of “empty calories”. The concentration of thiamine would be normal for a healthy calorie load, as would exist in an organic natural diet.
We have reported high calorie malnutrition as a common cause of this widespread disease. Dysautonomia is responsible for the symptoms because the hind brain, where the control mechanisms of the autonomic nervous system exist, is highly sensitive to cellular energy deficiency. It matters little whether it is called Beriberi or high calorie malnutrition as long as the biochemical cause is understood.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Ana Municio on Unsplash.