On and off over the last several years, I have had peripheral neuropathy along with a number of other strange symptoms like air hunger, light and sound sensitivity, and balance and gait issues that I believe are related to an undiagnosed thiamine deficiency.
Peripheral Neuropathy, Air Hunger, Dizziness, Altered Vision and Other Symptoms
I have always taken pretty good care of myself as well as taking supplements. I should note, that for the year prior to my health decline, I was drinking a lot of coffee, approximately 40-60 ounces per day. I have since learned that coffee diminishes thiamine. When I began to develop the neuropathy, I didn’t really know what it was. The strange sensations would come and go, but it became more and more intense in my legs and feet. Last summer, I also started to feel similar vibrations in my rib cage. It was extremely uncomfortable.
In addition to the neuropathy, I would wake up sometimes during the night gasping for air. Toward the end of last summer, I could really feel my energy slowly waning and in November of 2019, I had the flu. After I recovered from the flu, I still felt exhausted and weak. I went back to the doctor in December, 2019 and was found hypothyroid and put on Levothyroxine. I have been diagnosed with Hashimoto’s Thyroiditis. Anyway, I did not feel much better and I went back in January, 2020. I had a chest x-ray which showed lung inflammation and was told it could be COPD or asthma. I was asked if I had been smoking and I said it had been 35 years since I’ve smoked. (I am now 61.) At this point, I had some serious nervous system disorder signs, which I now think were the signs of both dry and wet Beriberi.
My symptoms had progressed to the point that I was extremely sensitive to light and sound and had extreme lightheadedness/dizziness. My vision plane was tilted to maybe like a 30 degree angle. My gait was weird at times and my balance was terrible. I received a general blood test and was also tested for Lyme disease, Lupus, RA and other autoimmune diseases, with normal results. They also tested my adrenal and parathyroid hormones and that came back normal. My body overall had this continuous buzzing type of sensation. I am normally social but felt so bad that I wanted to withdraw from people.
Was It Thiamine?
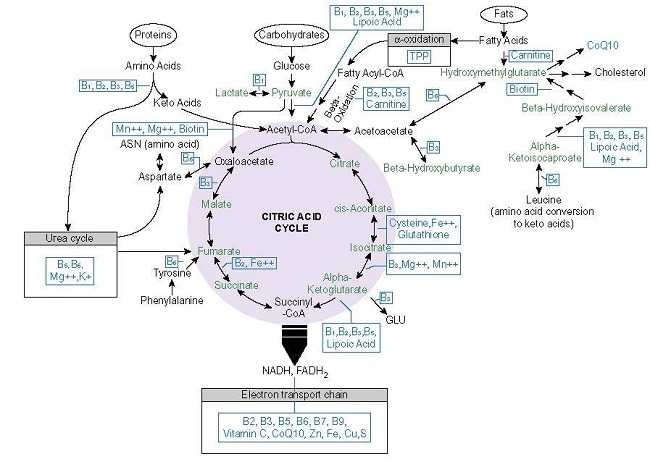
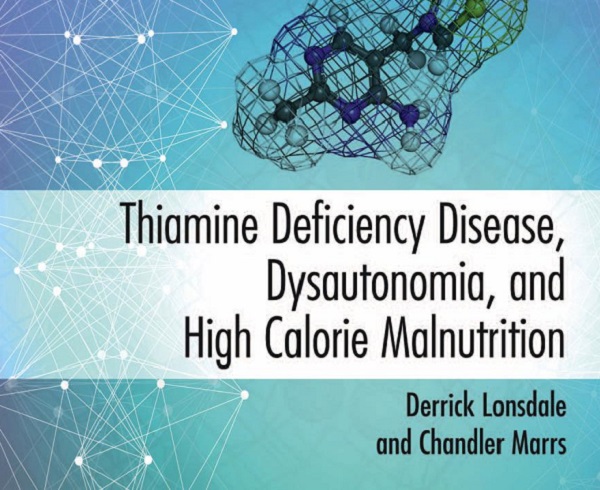
I found Drs. Lonsdale and Marrs information about thiamine and started on Allithiamine in mid-March 2020 and continued to see the chiropractor. I started with one, 50mg capsule per day and now am up to three 50 mg capsules a day. I plan on increasing to four capsules per day soon. The dizziness, balance problems, visual disturbances, light and sound sensitivity issues, and gait issues are pretty much gone.
What has worsened is that I have a hiatal hernia that never really bothered me that has begun to bother me a lot over the last 4-6 weeks. When I am having a flare-up, I am short of breath and my abdomen feels extremely tight between my ribs. This happens every few days. I feel that I have been healing but the abdominal discomfort and the effect it is having on my breathing is extremely uncomfortable at times. I am wondering if it is normal for one set of symptoms to resolve and a new set to arise. It is clear that the thiamine is helping with a number of my symptoms, the dizziness, balance and gait and the light and sound sensitivity have all improved, but the hernia and the pressure it causes on my breathing, has worsened. Will Allithiamine possibly help heal my lungs of the damage caused by smoking all those years ago? Will it help with the breathing and hiatal hernia or am I missing something?
I would love to hear your comments about all of this. I am deeply grateful for all of the work and research your site has done shedding light on the importance of thiamine.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Anja?#helpinghands #solidarity#stays healthy? from Pixabay