What does it feel like to have a stroke? We have all seen TV re-enactments of stroke and some of us have had the unfortunate opportunity to witness a stroke first hand, but few of us have any real sense of what a stroke feels like in the moments before it happens. Over the last several months, we have been investigating the early warning signs of birth control induced blood clots. Stroke survivors represent the largest group within our study so far. Their stories tell us a lot about the early warning signs of birth control induced strokes. Full stories can be read here, but since few have had any experience with stroke, especially birth control induced strokes, we thought it was important to highlight the key patterns.
Does It Hurt?
One of the more interesting questions, is there pain associated with a stroke? In some cases no, the stroke appears to come out of nowhere. In other cases, there is a clear progression of head pain in the weeks, days, and hours leading up to the event.
From no pain:
Right before the stroke – I was just really tired and crabby I went to take a shower and all of a sudden I felt really dizzy. I tried to get out and lay down but I fell out of the shower instead. I couldn’t tell anyone what was wrong because I couldn’t form any thoughts or words.
…head rush, as if I stood up to fast. No pain.
My left cheek had started to feel funny. It felt like when you went to the dentist and got Novocain and starts to wear off… an irritating numbness.
I was sitting down to tie my shoe and all of a sudden, my left hand wasn’t cooperating. It was banging against my shoe…I called for my husband but my words didn’t come out right. I tried to walk to him but collapsed on the floor…I didn’t feel any pain and definitely didn’t notice any symptoms prior.
I had trouble walking down the stairs…two days later, I became extremely confused and disoriented.
I got up to use the restroom. When I got back into bed, I couldn’t lift my right leg. I tried to wake my husband, but I couldn’t speak, so I shook him instead.
To paralyzing pain:
…The headache was extremely severe, almost paralyzing. Whatever song was playing on the television got trapped on repeat extremely loudly in my head…
I felt a pain that I will not soon forget strike through my right eye and up through my skull. It felt like a white hot bolt of lightning electrocuting my brain. The horizon was bouncing when I looked across the way. Worst migraine I’ve ever had for five days straight.
I had a headache that would not quit. I had worked all day and was going to a family wake. My headache was severe and my spouse looked at me and said I was going to the hospital.
I felt a sharp pain behind my left ear followed by an intense migraine headache with dizziness, falling, nausea and vomiting.
The Lead Up to Stroke: Early Unrecognized Symptoms
If birth control hyper-activates blood clotting, surely as clots progress in size and number, especially if they are in the brain, there would be symptoms? Indeed, there are. As women, however we tend to ignore our own health, and unfortunately, so too do our physicians. So even when the pain reaches an unbearable state, and we seek medical attention, it is often dismissed.
“I may have been having transient ischemic attacks for about six months prior to my stroke…I had been having episodes of dizziness and headaches leading up to my stroke. Since my stroke I have not had any of these episodes.”
One of my legs was swollen for a month before the stroke. My stroke started in the morning while I was at work. I have chronic migraines, and at first, I thought it was migraine. After work, I went home and rested. The symptoms kept getting worse, and when I tried to get up, I couldn’t walk.
The headache started a month earlier…I also had unexplainable pain in my left thigh.
Headache responded to Tylenol for five days. Wasn’t thinking it was a stroke. Vision blurry in one eye for a few days – assumed contacts needed changing or a new eye exam. Not until speech became impaired did we jump into action and rush her to the ER.
I had a burning and throbbing sensation in my head. It was not a headache. The sensation was felt from ear to ear, around the back of my head, across the center of the back of my head. I also felt the sensation on the right side of my head, close to my ear. I felt it for about a week in January (four months prior to the stroke), then it went away. The blurry vision started at the end of February (two months prior), and by March (one month prior), the burning and throbbing was constant – all day, every day.
Electrical shock sensation down my arm. Immediate dizzy spell…Tried to get dressed and my left hand didn’t understand that I was trying to grab my jeans of the bed. I went to work. Didn’t know that I had a stroke…I wasn’t diagnosed with a stroke for six months following. They assumed I had MS. The lesion on my brain looked like MS…
Clotting Disorders and Birth Control
One of the more striking patterns that we saw across all types of clot events, was the lack of recognition that hormonal birth control is contraindicated in women who have clotting disorders. None of the women in our study were tested for clotting disorders before being prescribed the contraceptive, even when there was a family history of clotting.
“I told my gynecologist that my father had had blood clots. She said, ‘That’s not a problem. The pill is only contraindicated if YOU had a blood clot.’”
Clotting disorders, it appears, are only ever recognized after one has a clot. For some women, this medical misinterpretation is deadly.
Missing the Clot
Over and over again, we saw symptoms dismissed or misdiagnosed. With impending stroke, the pain is often attributed to migraine, but as was indicated above, the pain was far and above that of a migraine.
The gynecologist told me the pain in my leg was probably just a muscle strain and she prescribed Imitrex for the headache…The migraine medication made the headache go from dull and persistent to unbearable…Over the next two days, I would take three ambulance rides, be sent home from the emergency room twice, begin to lose control of my body, and be given a very stern lecture from a nurse who thought I needed to learn how to ‘manage my stress’.
Since the medical staff at the ER originally thought it was a bad migraine, I received narcotics and Novocain shots in the back of my neck and the base of my skull to numb the muscles.
What Have We Learned?
The more stories we review, the more clearly we recognize that as women we don’t trust our intuition that something is wrong. This is often because our concerns have been dismissed by doctors in the past, or we fear that they will be. Except for perhaps those crises that happened suddenly, there were warning signs, sometimes seemingly innocuous warnings, but warnings nevertheless. Inevitably those warnings were put aside. As women, we are taught to be tough and plow through our health issues. We go to work, take care of our kids, our families, even when in excruciating pain. I think it’s time we learn to take care of ourselves first. If something doesn’t feel right, we need to trust our instincts, and be persistent in advocating for our own health.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on October 5, 2016. We subsequently lost funding to finish this study. Nevertheless, we are still accepting stories about birth induced blood clots. If you’d like to share your story, send us a note: Write for us. Other stories and articles about birth control and blood clots can be read here.
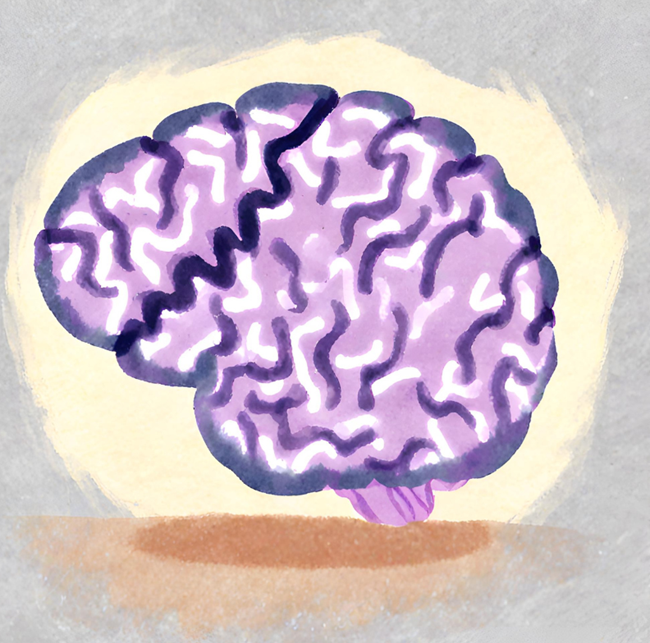
Image created in Canva with AI; property of Hormones Matter.