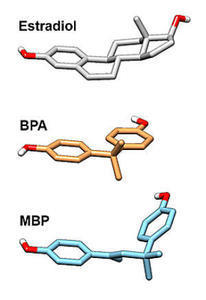
Bisphenol A or BPA is ubiquitous in the modern environment. Used to form plastics for array of products (and found in fracking waste water, as we just learned), BPA exposure is almost unavoidable these days. A study in 2008, showed just how unavoidable demonstrating high levels of BPA in 93% of the individuals tested. Like many environmental endocrine disruptors, BPA is estrogenic in nature. When exposure to environmental estrogens occurs during pregnancy or during early life, those estrogens affect male and female reproductive and neurological development significantly. Adding to the body of research against BPA and other estrogenic environmental endocrine disruptors (here, here, and here), a new study, Bisphenol A Promotes Human Prostate Stem – Progenitor Cell Self – Renewal and Increases in vivo Carcinogenesis in Human Prostate Epithelium links developmental BPA exposure to a significantly increased risk of prostate cancer for men later in life.
The study, conducted by researchers from the University of Chicago, Illinois, was rather unique in its approach. Researchers cultivated prostate stem cells from young, disease-free men and then conducted a series of both in vitro and in vivo exposure tests. In the in vitro tests they exposed the human cells, in culture, to the various levels of hormones over differing periods. With the in vivo tests, however, the researchers took those same human prostate progenitor cells and grafted them to host rats. The host rats were then exposed to the different hormones for different time periods. Hormones tested included: native testosterone, estradiol and BPA, the environmental estrogen that mimics native estradiol. In both series of experiments researchers were interested in the timing and length of hormone exposure on prostate carcinogenesis. What they found was striking.
Male prostate tissue, though dependent on testosterone for development, is also susceptible to native and environmental estrogens. Both types of estrogen receptors are present. Moreover, the timing and duration of estrogen exposure impacts prostate health health. Specifically, treatment of the host rodents for 1-4 months with native testosterone plus estradiol produced a relatively small incidence of cancer, only 13%. Treatment of the host rodents with BPA, however, increased the rate to 33-45%, with higher rates of carcinogenesis linked to longer exposures.
This study provides further evidence that early developmental exposure to environmental estrogens negatively affects male prostate health.
We Need Your Help
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
This post was published originally on Hormones Matter on January 10, 2014.