A recently published retrospective study showed ICU patients receiving thiamine therapy had a significantly reduced thrombosis and mortality rate compared to patients not treated with thiamine. The study, conducted in two hospitals in Saudi Arabia reviewed the cases of 738 critically ill Covid patients admitted to the ICU. As this was a retrospective study looking solely at electronic medical records, there was no determination of thiamine deficiency or clinical criteria to determine who received thiamine or at what dose. This was simply a review of all cases during a defined period of time that were admitted to the ICU and who, based upon clinical judgement of the treating physician, may have been prescribed thiamine.
Study Details
Among 738 patients, 83 had received IV or oral thiamine in doses ranging 50-200mg per day for an average of 7 days. This was in addition to whatever medical or pharmaceutical interventions provided. Using a statistical tool called a propensity score, the researchers then selected pair matches to those 83 patients for further analysis of several endpoints. The endpoints evaluated included:
- Association between thiamine use as an adjunctive therapy with in-hospital and 30 day mortality
- Duration of mechanical ventilation, length of stay and complications such as
- Acute kidney injury
- Thrombosis
- Respiratory failure
- Acute liver injury
Results
Across all variables, patients who received thiamine faired significantly better than those who did not. The most striking findings included mortality and thrombosis reduction. Thiamine reduced in-hospital and 30-day mortality by 61% and 63%, respectively compared to propensity matched controls. Additionally, critically ill ICU patients who received thiamine were 81% less likely to develop thrombosis, and non-significantly less likely to develop kidney damage or liver damage. Inasmuch as thrombosis is major contributor to mortality with COVID, this finding is huge.
Things to Consider
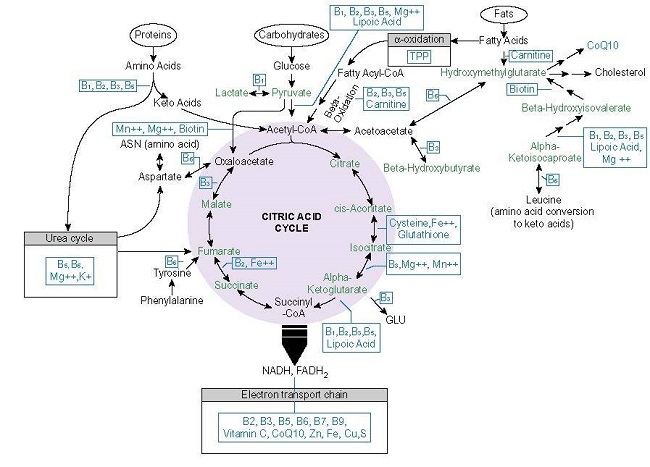
As this was a retrospective study and there were no determinations regarding deficiency or guidelines regarding dosing or other treatment protocols given concurrently, it is difficult to fully appreciate the role of thiamine in COVID recovery by traditional research parameters. Nevertheless, if we look at the role of thiamine in energy metabolism, in immune function, in controlling hypoxia, it makes sense that no matter what other confounding variables may detract from or enhance recovery prospects, thiamine, by its very mechanisms of action, would improve outcomes; something that we have been proposing since well before the pandemic began. Maybe now, more will listen.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.