Precocious Puberty
My daughter was recently diagnosed with precocious puberty and advancing bone age despite her short stature. At 6 years old, the endocrinologist estimated her bone age to be 11 years. She began her period in August, at age 8, weighing 63 lbs and standing only 4’4 tall. Our physician recommend the GnRH agonist Supprelin. After researching the side effects, I am concerned and have decided against using this drug. I am at loss, however, as to what to do. I am hoping someone with experience with precocious puberty will read this and offer suggestions beyond the drugs. Below is her health history.
A Baby Girl is Born
In January 2012, I gave birth to our beautiful and long awaited baby girl. My pregnancy was uneventful. I had a vaginal birth delivery but developed a complication right after her birth. I continued to bleed and required a blood transfusion the next day. During the transfusion, I developed a severe allergy to the plasma, and was given an Epi shot.
My daughter was 6lbs 5 oz at birth and healthy, however because I had to be taken to the OR to be stitched up and was given narcotics, I could not breastfeed and she was put on Similac. I continued to give her Similac, as I did not have a good enough output of breastmilk and stopped breastfeeding at two months. At the hospital they said her bilirubin level was a bit low and she went under some light for about half a day or one day. She was a very petite baby. At one month, she was 8lbs. The pediatrician did not seem concerned as I am also very petite.
Early Feeding Issues: Oral Dysphagia
In addition to the formula, I started Gerber oatmeal at around 4 or 5 months and she liked to have that cereal. At around 9 months, however, when I tried to introduce stage 3 foods, she started throwing up, as she tried to swallow the tiny pieces of food without chewing it. She refused to eat crackers and other food that required chewing. We continued to offer her pureed food. She also could not drink from a sippy cup, so after every meal I used to give her water in a spoon. The doctor said she may just need some time and to continue to try and offer her solid foods.
When she was around 4 years of age, we started on feeding therapy. The doctors said she has oral dysphagia and requires therapy. After about 6 months of therapy, she improved slightly, however still refused food that required chewing. Her diet at this time was mainly milk, cream of wheat, cheese, yoghurt, pasta, sweet potato puree, spinach, carrots and eggs. The doctor recommended Pediasure, so that was added to her diet as well.
We took her for feeding therapy again when she was 6 years old and the therapist told us that she needed to stop drinking milk from a bottle as it could impair her speech. When we switched to offering milk in a cup, she refused to drink milk. I was told not to force her to eat, as the therapist indicated that she appears anxious around food. Her diet expanded around the age of 7. She ate rice, quinoa, bread, lentils, more vegetables, and salmon. Occasionally she would eat chicken and beef it was very soft. The only food she eats from outside is the occasional cheese pizza or mac and cheese. She doesn’t like sweets, so no cookies, cake, candy, ice cream, sodas, juice etc. She also doesn’t really like any fast food. The only fruit she eats is bananas. I try to offer a banana at least once a day.
She hardly gets hungry, she never asks for food or water, which was concerning to me and I brought it up to the therapists. They did a physical exam and said she was okay. They said to increase fiber foods, and prescribed a laxative.
She continues to take a long time to eat her meals, on average dinner is around 2 hours. The lunch break in school is not enough for her to finish the sandwich (almond butter and jelly) that I send so most days when she comes home around 4.30PM she has hardly had any lunch. She finishes her sandwich at home, while I scramble to get her dinner ready, which she finishes quite late and just in time for bed.
At around age 7-8, she started eating bacon and hot dogs,. She doesn’t really like bacon that much but seems to like hot dogs.
Vaccines, Medication, and Medical History
My daughter is up to date on all her vaccines and takes the yearly flu shot. For a brief period in time, when she was 4 years old, she had asthma that was brought on by a cold and was prescribed Albuterol and Qvar. Her asthma cleared up very soon though and only appeared when she got sick with a cold, but that was also just a few times. Since then she has had many colds and not required any asthma medication. When she was 7 years old, she underwent a small procedure to remove a congenital nevus on her tummy that the doctor was a bit concerned about, however it was benign. She sometimes complains of stomach pains but I believe this is because of constipation. She doesn’t drink water unless I make her drink water.
Physical Activity
My daughter is not very physically active. I have to coax her to leave the house and that’s the only time she throws a tantrum. She prefers to play with her toys or video games and watch TV. She goes for swimming once a week, and in 2020 I enrolled her in yoga classes and circuit training classes but then COVID hit, so she could not attend many sessions. In school she has a PE class and does play with the other kids in the playground.
Early Signs of Precocious Puberty
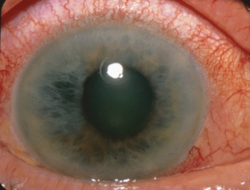
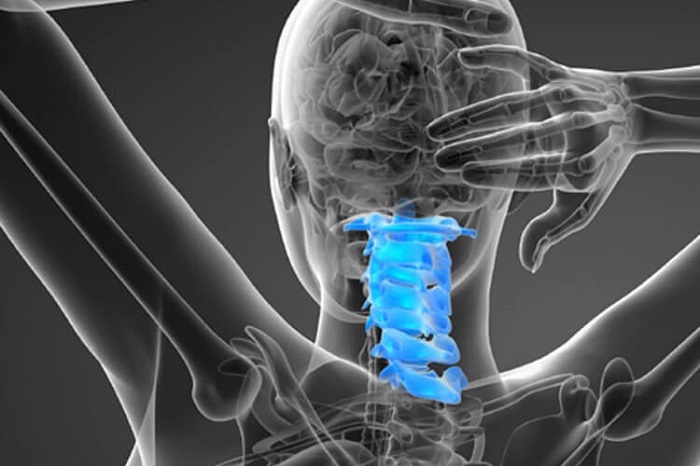
Around the age of 6 years old, I noticed breast buds poking through her shirt, I convinced myself that I was seeing things but took her to the pediatrician a few months later and she ordered a bone X-ray to determine if this was ‘early normal’ puberty. I got a call from the doctor indicating that her bone age was 11 and that she was referring us to a pediatric endocrinologist. The endocrinologist confirmed that bone age was 11 because of something that looked like a white circle on the X-ray near the thumb. She said that only appears at age 11. She also said that based on physical appearance that she may be at a tanner stage iii.
She wanted us to start on the supprelin implant right away, my daughter was then 7 years old. I did some research and saw that GnRH agonists have a lot of side effects and are used to treat cancer patients. My husband and I decided not to treat, as my daughter, even though she was aware that she was maturing, didn’t seemed bothered by it and was always happy and joyful. The thought of her having any of the side effects was too much to bear and we were happy with our decision.
I tried to look at natural ways to perhaps stop it and I found out that cows milk is loaded with hormones, so then I switched her to almond milk (in her daily cream of wheat) for about a year, but at the start of this year, I switched back to cow’s milk as she seemed to be losing weight and since she doesn’t eat well at school I didn’t want her to miss out on the calories.
Looking back, I think we were in denial because I was an early bloomer as well and I got my first period at 10.5 years old. I had early breast development as well but don’t remember the exact age my breast development started. I was around a B cup at the time of menarche (bigger than my daughter for sure). I was never tested for precocious puberty. I was a chubby kid and do remember developing earlier than my classmates. I don’t remember hair growth, but it was definitely present at the time of menarche. I also remember my mom telling her friends that I was the biggest kid in class, but that I suddenly stopped growing. I thought my daughter would be just like me.
Menarche At 8 Years Old
My daughter got her first period in August, at age 8, weighing 63 lbs and only 4’4 tall. She handled it well and this did not seem to bother her at all, however by the 3rd day she wanted to know when it will stop. Her cycle lasted four days.
It has been quite a shock to me because I thought she’d get her period at 10 like me. All I’ve been doing since is Googling, and Facebook messaging anyone who may have gone through something similar with precocious puberty. Almost every article I read indicates that there is not much growth left and that growth plates close at bone age 14 or 15. In my daughter’s case I’m guessing her bone age is 13, given it was 5 years advanced when she was 6. I suspect her tanner stage looks to be around IV based on physical appearance. I don’t know how tall my daughter will end up at. She is her usual happy and cheerful self, but I am a wreck. I am only 4’11.5 and my husband is 5’7.5 so I know she may not be that tall but I’m hoping she can at least reach 4’7 or 4’8. My daughter is otherwise healthy.
Potentially Relevant Family Medical History
I have a history of ovarian dermoid cysts. I have had two surgeries; one in 2005, the other in 2017. I have only been pregnant once. Last year I was diagnosed with pre-diabetes and I’ve been trying to clean up my diet. I also have fatty liver (liver function tests are normal) and gallbladder stones (I’m 37). I had to see a hematologist prior to my dermoid cyst surgery in 2017 because the doctor was worried that I might have a bleeding condition. The hematologist, after a battery of tests, said he thinks I have some kind of bleeding issue but that it’s not severe. He did prescribe iron supplements for 6 months. I was also found to be deficient in vitamin D and I was prescribed 50000IU of Vitamin D2 once a week. I think I had to take this for about 2 months.
My husband’s sister started her period at age 9 and is currently 5’3 tall. I am unsure if this was a case of precocious puberty, as she was not shown to a doctor either. She does remember being taller than the rest of her peers in school. She was overweight as a kid.
Early puberty is somewhat common in the South Asian region that we originate from. I remember quite a few of my friends getting their periods at 9 or 10. No one ever goes to the doctor to get checked, so this bone age concept is new to me and I am very worried on how it would impact final height.
Where We Are Now
I’m on the lookout for some nutritional supplements that would help her grow, but not cause further acceleration that could cause her growth plates to close as I feel I failed her already and do not want to do anything that could impact her final height negatively. I read that physical activity can increase growth hormone, which I really did not know before this, so I now make her run outside and do some physical activity daily. I’m meeting with another endocrinologist this week to determine impacts to final height. I really don’t want to treat her with puberty blockers, but I’m worried she will end up very short and blame us for not treating. I did come across some other parents whose kids started menarche at 8 or earlier who grew around 5 – 6 inches without treatment, however their bone age was not as advanced as our daughter’s, so I worry that she may not have that same level of growth.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Rudy and Peter Skitterians from Pixabay.
This article was published originally on August 17, 2020.