Yes, and increased use of environmental toxicants may be partially to blame. Over the last decade researchers have uncovered connections between tissue level vitamin A activity – the retinoic acid pathway – hormone metabolism, and the cell cycle overgrowth noted in fibroid tumor development, breast and ovarian cancer, and endometriotic tissue growth. Moreover, researchers from the environmental side have found that the popular glyphosate-based herbicides alter vitamin A or retinoic acid metabolism which in turn alters androgen and estrogen metabolism. Connecting the dots, we may have a first step to reducing cell growth in these conditions; remove the toxicant exposure and increase nutritional resources. A second step may be to develop locally absorbed vitamin A, applied directly to the aberrant tissues.
What is Vitamin A?
Vitamin A, (retinol, carotene) is a fat-soluble nutrient that we derive solely from dietary sources. It is responsible for a myriad of functions in a vast number of tissues from the eye, to the ovary, to the heart. Historically, nutrition from diet, coupled with the old wives’ tales of good health, carrots for eyesight, and cod liver oil for all that ails you, were all that were needed to maintain healthy levels of Vitamin A in most individuals. However, with the increase in processed foods, modern farming, intense use of herbicides and pesticides, and the general replacement of the old wives’ nutritional wisdom with pharmaceuticals, many men, women, and children are vitamin A deficient and likely do not even know it. The WHO estimates vitamin A deficiency in 19 million pregnant women and 150 million children worldwide. When Vitamin A deficiency reaches its nadir night blindness, maternal mortality, and difficulty fighting infections are common. In women, the first signs of vitamin A deficiency may be unrecognized and include fibroids or endometriosis. Earlier signs of vitamin A deficiency in women could also be menorrhagia (heavy menstrual bleeding) that often precedes fibroid or endometriosis diagnosis, but research is lacking here, or even genital warts of the common HPV strains.
Why Retinoic Acid, Hormones, and Cell Growth
Retinoic acid (RA), is the form of vitamin A stored in the body. RA is what is called a paracrine, perhaps even an intracrine hormone regulator. That means it turns hormone metabolism on or off in the cells within its immediate vicinity (paracrine) or within its own cell (intracrine). This is compared to endocrine control of hormone metabolism – where hormones and the factors that regulate hormone synthesis and metabolism travel vast distances through the blood to reach their targets tissues (the hypothalamus-pituitary – ovarian system is an example of endocrine regulation) or autocrine where the hormone leaves its own cell only to turn around and bind to a receptor on that cell. In contrast, retinoic acid stays close to home and regulates local cell behavior, both internally and proximally. The vitamin A deficiency leading to fibroids or endometriosis represents a cell and tissue level disruption of the retinoic acid pathway that in turn interrupts the normal cell cycle (differentiation, proliferation, and apoptosis -cell death) and elicits all sorts of problems from decreased estrogen metabolism (too much estradiol at the cells), to cell overgrowth, or more specifically, not enough cell death where needed. The results include aberrant cell growth as in fibroids, tumors, and endometriosis.
Retinoic Acid, Progesterone and Estrogen Metabolism
With many women’s health conditions too much estradiol at the tissue level is at the root. Estradiol is an excitatory hormone that tells our cells to go forth and prosper. Progesterone, depending upon the tissue and the relative values of each circulating hormone can work synergistically to enhance estradiol’s actions or it can shut it down entirely via the upregulation of a specific estradiol metabolizing enzyme called 17 beta-hydroxysteroid dehydrogenase type 2 (17B -HSD2). When these enzyme levels are high, more estradiol is converted to estrone. Since estrone is a less potent estrogen than estradiol, metabolism of estradiol to estrone somewhat inactivates the estrogen and slows cell proliferation. When the enzyme levels are low, more estradiol remains, and cell growth is enhanced. Vitamin A or retinoic acid mediates the progesterone-dependent activation of this enzyme, effectively regulating estradiol concentrations locally. Too little retinoic acid or a disrupted retinoic acid pathway and estradiol is not converted to estrone – e.g. it is not inactivated. Cell proliferation dominates, while normal cell death or apoptosis is reduced. Fibroids, tumors, or endometriosis ensue.
What Causes Low Retinoic Acid or Reduced Functioning?
Vitamin A is derived entirely from diet. Foods high in vitamin A include brightly colored vegetables, dark leafy greens, carrots, pumpkin, sweet potatoes, bell peppers, and fatty fish oils, like cod liver oil and organ tissues like the liver. Meat and dairy also have high concentrations of vitamin A. Diets high in processed food do not contain sufficient vitamin A to maintain the proper cell cycle balance and so we get too much proliferation and too little apoptosis. Tissues grow and grow and do not die.
Alcohol intake reduces the body’s ability to metabolize retinoic acid because alcohol and the retinoic acid pathway use the same enzymes – alcohol dehydrogenase (ADH1) and aldehyde dehydrogenase (ALDH1) for metabolism. Alcohol competes for the enzyme and so vitamin A from diet cannot be converted to the usable retinoic acid.
Can Toxins Disrupt the Vitamin A Pathway?
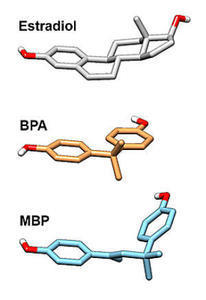
Yes, but here is where it gets complicated. Environmental toxins like glyphosate used in common weed killers such as Round-up have a complex relationship with the vitamin A pathway and hormone metabolism. These herbicides and many pesticides are endocrine disruptors, meaning they disrupt ‘normal’ hormone metabolism, often towards a hyper-estrogenic state. Similarly, plastics like BPA and a host of industrial chemicals are also endocrine disruptors that move us towards hyper-estrogenism – a key component of fibroid and endometriosis.
Glysophate activates an enzyme called retinaldehyde dehydrogenase which increases retinoic acid synthesis. This is argued to be the mechanism by which environmental exposures during pregnancy cause birth defects. However, glyphosate also inhibits vitamin A metabolism by a similar mechanism as alcohol, by competing for ADH1 availability, thereby having the ability to reduce vitamin A synthesis. Glyphosate also increases aromatase activity (the enzyme that converts testosterone to estradiol), creating a hyper-estrogenic state and depending upon the time course and the exposure concentration, completely wipes out aromatase activity. So like any true hormone system, that uses a complex chain of compensatory reactions to maintain homeostasis, the reactions to environmental toxins are complicated and non-linear. Nevertheless, they warrant attention, particularly when one is suffering from a condition affected by the environmental toxin in question.
Managing Vitamin A Levels
To determine if you are vitamin A deficient, seek out a lab that specializes in micronutrient testing. The recommended daily values of vitamin A can be found in the Dietary Supplement Fact Sheet.
Vitamin A is a fat-soluble vitamin, meaning that it will be stored in fat, and toxicity from too much vitamin A is possible. It is rare, but nevertheless, if supplementing, vitamin A levels should be monitored by micronutrient testing.
My Two Cents
Much of the research presented here linking local vitamin A deficiencies with endometriotic, fibroid, and cancer growth has not crossed over into clinical care. Moreover, it is complex and far from settled. Except for cancer trials, mostly in males and mostly with oral supplementation, the research regarding dietary vitamin A is limited and mixed. However, I think a local application of an absorbable form of vitamin A or retinoic acid should be investigated for the treatment of endometriotic and fibroid growth in women. Similarly, dietary supplementation within acceptable levels and changes combined with environmental ‘cleaning’ may be of use, if only to improve the overall health status of women currently suffering from fibroids or endometriosis.
Postscript: This article was published previously in August 2013.
Photo by Tamanna Rumee on Unsplash.










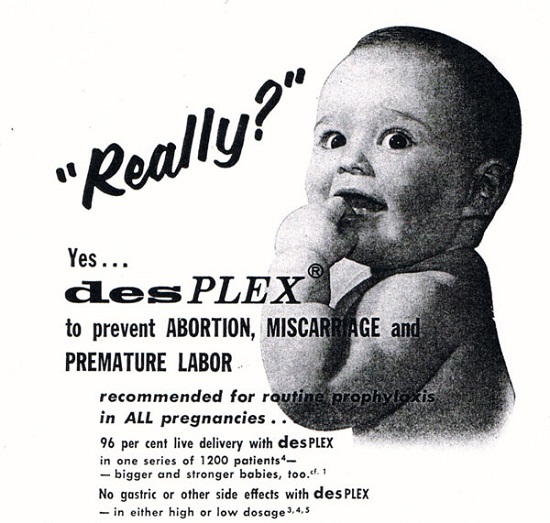
 DES is not something of the past. People who have been exposed to this drug years ago are battling with health issues and fighting for their lives as I’m writing this blog post. Who knows what health problems the grandchildren of the mothers who were prescribed this drug will have to deal with as they grow up. I want my daughters to receive adequate medical care and monitoring if they ever have to suffer the consequences of this drug. This is why together with my husband we support the great work done by the very few International DES Action Groups who are providing valuable information and are advocating for the DES victims.
DES is not something of the past. People who have been exposed to this drug years ago are battling with health issues and fighting for their lives as I’m writing this blog post. Who knows what health problems the grandchildren of the mothers who were prescribed this drug will have to deal with as they grow up. I want my daughters to receive adequate medical care and monitoring if they ever have to suffer the consequences of this drug. This is why together with my husband we support the great work done by the very few International DES Action Groups who are providing valuable information and are advocating for the DES victims.