In 2011 a mother called me and asked whether I would be able to help her 14-year old son who had been diagnosed with eosinophilic esophagitis. Because this disease had only been recognized in the past two decades I had to confess that I had never heard of it. Because I used only nutrients in therapy, I confessed my ignorance but that I was willing to have a shot at it. Obviously, the first thing that I did was to see what had been written about this newly recognized condition.
Eosinophilic Esophagitis: Inflammation of the Esophagus
The part of the gastrointestinal tract that is most commonly affected by this inflammatory infiltration is the esophagus (esophagitis), although it has been recorded in other parts of the intestine when it is known as eosinophilic enteritis. Eosinophils are specialized white cells that have a role in inflammation. They have this particular name because they stain with a dye called eosin (the postfix phil is derived from the Latin word for love) making it easy for a pathologist to recognize their presence in tissues.
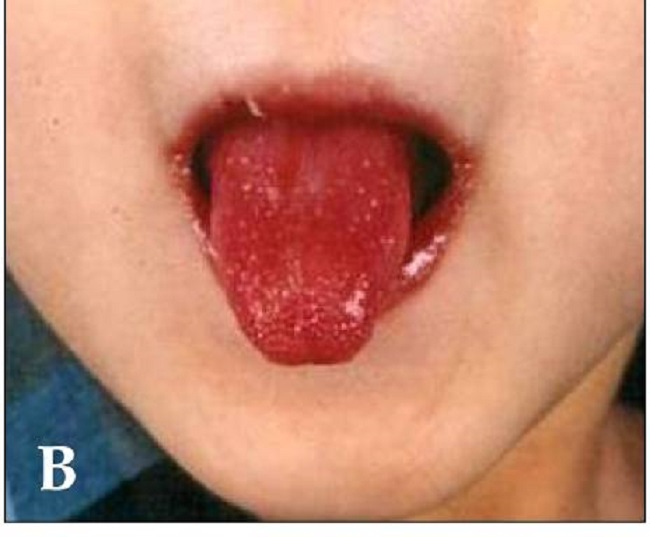
Eosinophilic esophagitis (EoE) is now by far the most common form of eosinophilically infiltrated gastrointestinal disease. It represents the most recent form of food allergy, and its control by avoiding offending foods has increasingly appeared as a therapeutic approach. It is often poorly responsive to therapy and there is no commonly accepted long-term treatment. The diagnosis has to be made by endoscopy and it is distinguished from other causes of inflammation by finding eosinophils in the inflammatory area.
A Complex Medical History Misdiagnosed As Psychosomatic
The medical history of this 14-year-old boy had begun in infancy with recurrent ear infections and asthma, entailing many doctor visits. But he also had many confusing symptoms throughout childhood other than the chest pain and swallowing difficulties that might be expected from inflammation of the esophagus. In fact, these symptoms had been thought of as psychosomatic until endoscopy was performed when he was 8 years old and the esophagitis was discovered. From that time on, he had been examined repeatedly and had received conventional treatment without success at several prestigious institutions. He came to my attention 6 years after the diagnosis had been made.
His early history of repeated ear infections and asthma were important because both of these conditions are now known to be related to inefficient oxidative metabolism. Eosinophils are associated with asthma in some cases. The symptoms that had been considered to be psychosomatic included a dramatic response to any physical pain producing stimulus (hyperalgesia), emotional instability, unusual fatigue, headaches, dizziness, panic attacks and increased sensitivity to both sound and light. For example, when I came to the physical examination he would scream when I touched his abdomen and the abdominal muscles would become rigid. Another intriguing symptom was that he coughed in his sleep (an exaggerated cough reflex) without becoming awakened and he also experienced nightmares. He had also been diagnosed by a psychologist with ADHD and OCD. But on physical examination, I also found many intriguing signs that indicated autonomic nervous system dysfunction. The medical history also indicated that he was addicted to sugar, and alcoholism was widespread on both sides of the family, both being related to thiamine metabolism. People who have read some of the posts on this website will be familiar with the association of thiamine deficiency with sugar ingestion and alcohol.
A Family History of Alcoholism and Thiamine Metabolism
Because of this family history of alcoholism, his addiction to sugar, and the known relationship of thiamine deficiency with autonomic dysfunction, I used the blood test known as erythrocyte transketolase and I was not too surprised to find that it was extremely abnormal, proving a severe degree of thiamine deficiency or abnormal thiamine metabolism. He was treated with a series of intravenous infusions of water-soluble vitamins that contained thiamine hydrochloride. Although his symptoms began to improve, the transketolase test became much more abnormal, suggesting that thiamine was not being absorbed into the cells that needed it. Thiamine tetrahydrofurfuryl disulfide (TTFD: Lipothiamine, a derivative of thiamine that is absorbed more easily because it does not require the complex mechanism that is required for the absorption of dietary thiamine) was substituted for the thiamine hydrochloride with the result that the transketolase improved greatly.
Symptoms continued to improve but the most surprising thing that happened was the tremendous growth spurt that occurred throughout a year of treatment. Body weight at the beginning of treatment was 105 pounds, placing him in the 25th percentile. After one year of treatment his weight had increased to 122 pounds (+17#), placing him in the 50th percentile (e.g. male or female members of a school class). His stature increased in the same time period from 64.5 inches to 68.5 inches (+4”), raising it from the 50th to the 75th percentile. Percentiles are used in growth charts to indicate the normal height and weight of an individual as compared with subjects of the same age. For example, the fiftieth percentile would mean that 50% of a given similar group (e.g. a school class) would be taller/heavier and 50% shorter/lighter. For normal height and weight a subject remains in the same percentile throughout growth. A “jump” of this nature is extremely rare. It is unlikely that he would have been considered growth retarded if this dramatic acceleration had not occurred. He would have just been regarded as a “shorty”.
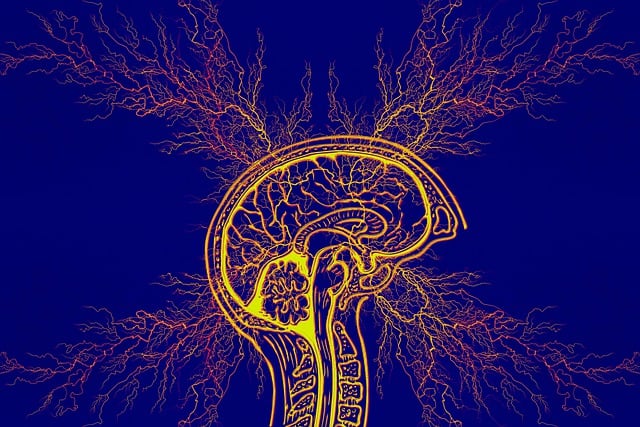
Dysautonomia
As reported in several posts on this website, dysautonomia is used to describe changes in the functional controls of the autonomic (automatic) nervous system. There are two branches to this system known as sympathetic, the action system, and parasympathetic, the “rest and be thankful” system. The first one is activated by any form of stress that includes a mild degree of oxygen lack (hypoxia) in the lower part of the brain or its equivalent from lack of thiamine and known as pseudohypoxia. There is also a genetically determined disease known as Familial Dysautonomia (FD) in which growth retardation is a constant feature. Although FD is a genetically determined disease, it is the resulting dysautonomia that causes growth failure. This suggests that the long-standing dysautonomia in this patient, due to energy inefficiency in brain cells caused by the pseudohypoxia of thiamine deficiency, was responsible for growth failure. Restoration of thiamine concentrations caused improvement in energy metabolism that enabled the growth spurt to take place.
Conclusion: Inflammation Is a Defensive Response
Inflammation is really a defensive response made by the body to some form of attack. In the case of this disease it appears that certain foods act as the attacking agent, hence the term food allergy. The inflammatory reaction is kept under very careful control by the brain acting through a nerve that runs the entire length of the intestinal tract. If this nerve fails in its suppressive action, the inflammation gets out of control. For the normal function of this nerve thiamine is a necessity. But thiamine deficiency, because it results in pseudohypoxia, also activates the sympathetic branch of the autonomic system and was responsible for the many symptoms that had been previously described as psychosomatic. It is very likely that the huge ingestion of sugar in the United States is responsible for thiamine deficiency that results in manifestations of disease that vary in their presentation according to the particular cells affected by the deficiency. Because of the family history I strongly suspect that there was a genetic relationship that created this boy’s sensitivity to foods, particularly sugar, making thiamine deficiency much more likely. It is of course possible that this is but one cause of eosinophilic esophagitis/enteritis. It suggests however that some form of pseudohypoxia (other than thiamine deficiency) is the root cause of the disease and that the inflammatory response gets out of control because of autonomic dysfunction. This case is now “in press”.
Lonsdale D. Is Esosinophilic Esophagitis a Sugar Sensitive Disease? J Gastric Disord Ther 2016;2(1):doihttp://cbcdoi.org/10.16966/2381-8689.114.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Myriam Zilles on Unsplash.
This article was published originally on February 8, 2016.