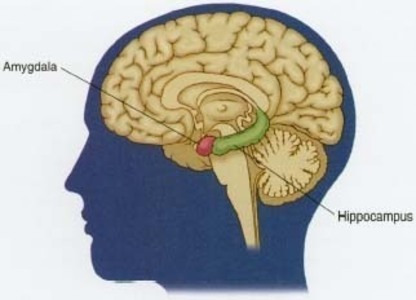
New research, conducted on rodents, suggests that pre-menopausal hysterectomy with ovariectomy induces changes in the hippocampus (memory center of brain) making it hypersensitive to ischemic stressors (reduced blood flow). In contrast, ischemic stressors did not cause hippocampal damage in non-ovariectomized female rats or even gonadectomized male rats
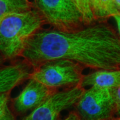
The hippocampus, located in the temporal lobe of the brain, is responsible for working memory formation, storage and retrieval. Researchers have long known that damage to cells in the hippocampus cause significant problems in short-term, long-term and working memory, ranging from mild cognitive decline to complete impairment. Certain cells in the hippocampus are particularly sensitive to the amyloid protein buildup associated with Alzheimer’s disease.
In the current study, removal of the ovaries and the associated long-term estradiol deprivation made the hippocampus hypersensitive to ischemic stressors and induced a myriad of events leading to significant hippocampal CA3 cell damage and cell death. The long term estradiol deprivation also led to increased amyloid production and associated neurodegeneration. As one might expect, damage and disruption to the hippocampus, the brain’s memory center, was associated with the animal’s ability to learn, remember and function.
What was particularly interesting, female animals who retained their ovaries and were exposed to the same ischemic stressor demonstrated neither the brain damage nor the decline in cognitive function. Similarly, male animals whose gonads were removed, suffered no notable brain damage or cognitive decline either. It was only the female animals whose ovaries were removed and whose systems were deprived of estradiol for a long period of time.
When estradiol was added back to the ovariectomized female animals shortly after the surgery, the female animals were able to weather the ischemic stressor and hippocampal damage was reduced significantly. However, when the estradiol was added back after an extended period of deprivation, it had no effect on the hippocampal damage or subsequent decline in memory.
Estradiol is important for cognitive function.
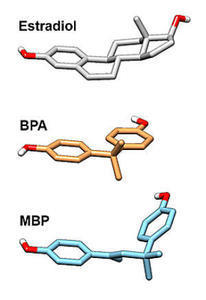
It is important to note, that animal researchers use 17B-estradiol, the same form of estradiol produced in the ovaries. In contrast, researchers who study human memory, often supplement with synthetic estrogens (Premarin, Prempro etc.), which is molecularly different than what is produced in our bodies. Indeed, the synthetic estrogen is actually about 20 different estrogenic compounds synthesized from pregnant horse urine. With synthetic hormone replacement therapy (HRT), recently renamed menopausal hormone therapy (MHT), the difference in molecular structure, as well as the long chain of metabolites that MHT produces, lead to an increase in the number of illnesses and may or may not be protective against the diminished estradiol induced hippocampal damage or the associated cognitive decline.