Fibromyalgia (FMS) is a complex chronic condition characterized by allodynia, pain, stiffness, paresthesias, and tenderness of the muscles, skin, and soft tissues. It also may feature HPA-axis dysregulation, circadian abnormalities, fatigue and muscle weakness, depression, and insomnia. Biochemical abnormalities include elevated markers of system oxidative stress, inflammation, and mitochondrial dysfunction. Many in the FMS community have achieved great successes using high doses of thiamine.
Covering all the underlying drivers of this condition is way beyond the scope of this article, because there are many. Instead, I will focus on the key neurological and metabolic abnormalities to explain the potential mechanisms by which thiamine can be useful.
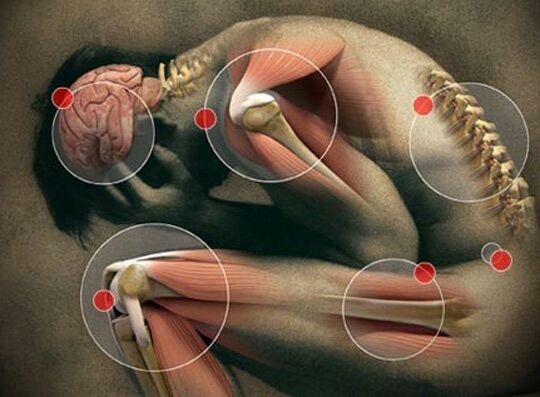
To understand how thiamine supplementation might help to resolve chronic pain, we must first cover the basics of pain signaling and examine which processes become dysfunctional in FMS. On the one hand, there are researchers who hypothesize that FMS originates in the central nervous system and is produced by changes in the way that the brain processes sensory information. Alternatively, other research highlights peripheral changes in the structure and metabolic function of tissues which likely also contribute to the sensation of chronic pain. In short, it appears that the causes of this condition are multifactorial and systemic.
Central Pain Processing
The medical term for sensing pain is nociception, and this can be divided into two opposing “branches” or pathways which either exert a facilitatory or inhibitory effect on pain sensing – pro-nociception and anti-nociception.
Without going into significant detail, pain sensing begins with sensory information detected by neurons in the peripheral tissues, which is then carried to the dorsal horn of the spinal cord. At the neuronal synapse, excitatory neurotransmitters such as glutamate are released and activate NMDA receptors to propagate a signal through the spinothalamic tract to a brain region called the thalamus. The stimulatory effects of these excitatory neurotransmitters can be amplified by another neurochemical named “substance P”, which in turn is also increased by Nerve Growth Factor. From the thalamus, the information is processed in other locations of the brain including the somatosensory cortex. Together, these processes constitute pro-nociception or “pro-pain” signaling.
On the other hand, signals from other brain areas descending through the brainstem reach the dorsal horn and act to oppose, inhibit, or modulate the magnitude of the pronociceptive signal. Hence, this is referred to as anti-nociception and serves an essential counterbalance function to prevent excessive or unopposed pain. The inhibitory action of anti-nociception is mediated through the biogenic amines norepinephrine (noradrenaline), serotonin and dopamine, along with other neurochemicals including the endogenous opioids.
An easy way to conceptualize this system is as though there were an “on” and “off” switch for pain. A well-working system is balanced between pro- and anti-nociception so that pain is perceived in the way that is appropriate to the context – neither too excessive nor too weak. If the pathways involved in pro-nociception were to overwhelm the counterbalancing effects of anti-nociception, or alternative if the neurochemical mediators involved in anti-nociception were too weak, the result would be chronic allodynia (the sensation of pain which is disproportionate to the stimulus). In other words, someone would feel chronic and excessive bodily pain for no apparent reason.
Unsurprisingly, research indicates that patients with FMS exhibit both of the above defects in central pain processing. Chemical mediators involved in pro-nociception have been shown to be abnormal in FMS. In the cerebrospinal fluid, pain enhancing chemicals substance P and nerve growth factor were both elevated. Brain insula levels of the excitatory neurotransmitter glutamate were also higher during pain. More recent data has identified elevated concentrations of glutamate in several areas of the brain, which is positively correlated with pain scores. Furthermore, increased glutamate levels in the posterior gyrus positively correlated with depression, pain, and global function in another study. Increased sensitivity of spinal neurons occurs in FMS, rendering them more susceptible to excessive stimulation of NMDA receptors by increased levels of glutamate. The resulting neuroexcitoxicity may be responsible for chronic hyperalgesia.
On the other hand, metabolites of other neurochemicals (the biogenic amines) involved in the inhibitory pathways were found to be lower in cerebrospinal fluid of patients with FMS. Furthermore, fMRI studies have demonstrated abnormal functional connectivity of the periaqueductal grey, a region of the brain involved in pain processing. Together, these findings support the notion that the portion of the central system involved in modulating pain may become dysfunctional – where pro-nociception (the “on-switch”) could be enhanced and anti-nociception (the “off-switch”) may be inhibited.
Mechanisms in the Hyper-excitable Brain
More recently, microglial activation was demonstrated in multiple brain regions involved in pain processing including the dorsolateral prefrontal cortex, dorsomedial PFC, primary somatosensory and motor cortices, precuneus, and posterior cingulate cortex. These findings are also suggestive of immune system activation and chronic neuroinflammation.
Another region of the central nervous system involved in pain processing is the dorsal root ganglia. This tissue is comprised of nodules positioned along the spinal column which key roles in pain signaling from the peripheral to the central nervous system. The ganglia are essentially made up of bundles of sensory nerve fibers which are tasked with conveying information to the higher centers in the brain.
Ordinarily dorsal root ganglia have minimal sympathetic innervation, although under the circumstances of acute trauma or infection (or under the influence of elevate nerve growth factor), sympathetic neurons in this region undergo a form of neuroplasticity called “sprouting”.
Sprouting increases the network of interconnections between sympathetic neurons and features a “hyper-excitability” of the sodium channels, where catecholamines and other sympathetic mediators induce sensory neuron firing. These mechanisms make up the basis for the concept of “sympathetic-driven-pain”, where activation of the sympathetic nervous system increases the sensation of systemic pain.
What this means is that the ordinary neurochemicals needed within the sympathetic nervous system can go on to stimulate hyper-excitable sensory cells in the DRG, and this produces the sensation of pain. It also means that inhibiting the hyper-excitability of these neurons is likely capable of reducing the perception of pain. DRG hyperexcitability is considered by some researchers to be one of the primary drivers behind the pain and dysautonomia in FMS. A genetic polymorphism (SCN9A) in the gene which encodes dorsal root ganglia sodium channels which is thought to contribute to hyperexcitability has been associated with severe FMS. Alterations in sodium channels and hyperexcitability of sensory neurons in the DRG likely plays a key role in the pathogenesis of a condition small fiber neuropathy.
This condition leads to degeneration of unmyelinated C and A-delta sensory neuron fibers and produces symptoms which are remarkably similar to those of FMS. It constitutes one of the main forms of diabetic neuropathy but can also be caused many other factors including autoimmunity and infection.
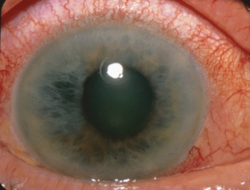
In fact, several lines of research have identified evidence of small-fiber neuropathy in FMS. Up to 30% of patients were shown to have abnormal epidermal nerve fiber density in the calf and skin. Two studies showed evidence of neuropathy using corneal assessment (here and here), and SF-neuropathy was also confirmed in 6 of 20 patients by another group of researchers. Patients with FMS were also found to have hyper-excitability of nociceptors on sensory neurons which closely resembles small fiber neuropathy. These findings have led some authors to hypothesize that idiopathic FMS may actually be undiagnosed small fiber neuropathy in a significant percentage of cases.
Aside from the factors discussed above, numerous research studies have identified a variety of other structural and functional abnormalities in the peripheral muscles and tissues of patients with FMS.
Mitochondria and Metabolism in Fibromyalgia
Research into FMS has demonstrated mitochondrial dysfunction in muscle tissue, skin and white blood cells. Muscle biopsies have identified mitochondrial changes such as irregular cristae, defects of cytochrome-c-oxidase, and deletions of mitochondrial DNA. There is also a decrease in enzymes involved in energy metabolism including citrate synthase, 3-hydroxyCoA dehydrogenase, and cytochrome oxidase. Evidence of this has also been found in skin biopsies.
In a brilliant paper titled “Metabolic Connection of Inflammatory Pain: Pivotal Role of a Pyruvate Dehydrogenase Kinase-Pyruvate Dehydrogenase-Lactic Acid Axis”, the authors emphasize the central role of cell metabolism in preventing or promoting chronic inflammatory pain. One consequence of defective oxidative respiration in cells is a “metabolic shift” away from using oxygen and toward anaerobic metabolism.
The mitochondrial enzyme responsible for transforming pyruvate (pyruvate dehydrogenase) becomes inhibited, and pyruvate is instead shunted down an alternative pathway to yield lactate as a “back-up route” to maintain energy flow. This not only reduces cellular ATP by a great amount, but the resulting tissues acidity may contribute to pain hypersensitivity through sensitizing peripheral pain receptors. It has been proposed that mitochondrial dysfunction may actually be a prerequisite for the development of pain in FMS. This was reflected in one study which found much greater interstitial and plasma concentrations of lactate in patients with chronic widespread pain/FMS. Importantly, the concentration of lactate correlated with pain thresholds and pain intensity – demonstrating a link between disturbed oxidative energy metabolism and chronic pain. Dysfunctional mitochondria are known to spew out excessive reactive oxygen species as a consequence of inefficient or “dirty” oxidative respiration. These ROS can go on damage important cell components and yield free radical species which, if left unchecked, produce a state of oxidative stress. The endogenous antioxidant enzymes and other antioxidant nutrients are responsible for combating the burden, but are limited in this capacity when the burden is becomes too heavy.
Excessive reactive oxygen species are likely involved in chronic pain via several mechanisms. Elevated spinal ROS was shown to induce central sensitization and pain without peripheral nerve injury. Superoxide is also capable of altering nociception to increase pain, and increased tissue levels of ROS have been demonstrated in animal models of chronic pain disorders. This is supported by research showing anti-nociceptive/analgesic effects of superoxide scavenging antioxidant formulations.
In line with this reasoning, the research indicates that oxidative stress is indeed a common finding in FMS. Antioxidant enzymes glutathione reductase, glutathione peroxidase, and catalase were shown to be significantly lower in FMS; along with higher markers of oxidative stress such as lipid peroxides and protein carbonyls. In that study, oxidative markers were correlated with symptom severity. Another group of researchers demonstrated similar results, also finding elevated markers of DNA damage when compared with controls. The skin of FMS patients was depleted in coenzyme Q10 and contained higher levels of malondialdehyde and expression of 8-oxoguanine glycolase, indicating oxidative DNA damage. A further study found increased protein peroxidation, a reduction in antioxidant thiol compounds, and depleted levels of nitric oxide.

Increased tissue concentrations of lactate stemming from localized mitochondrial dysfunction also promote a local inflammatory environment through triggering the release of cytokines IL-1B and TNF-a, along with increasing NF-KB-dependent inflammatory gene expression. Indeed, markers of systemic inflammation have been identified in FMS such as increased salivary and serum TNF-a, along with skin biopsies. Notably, TNF-a levels were positively correlated with pain scale scores, and negatively correlated with mitochondrial-DNA. Additionally, neurogenic inflammation (initiated by the nerve cells) is also associated with FMS. To summarize some of the key findings, FMS features:
- Defective central pain processing characterized by enhanced pro-nociception and reduced antinociceptive mediators
- Glutamate excitotoxicity in the central nervous system
- Neuroinflammation initiated by microglial cells
- A subset of patients display signs of small fiber neuropathy likely involving hyperexcitability of neurons in the dorsal root ganglia
- Mitochondrial dysfunction in skin, muscle and white blood cells
- Structural mitochondrial abnormalities
- Elevated tissue concentrations of lactate and pyruvate
- Elevated systemic inflammatory markers
- Elevated markers of oxidative stress with depleted endogenous antioxidant systems
So now that we have rough idea of how the system malfunctions in FMS, we can begin digging deeper into the ways in which thiamine can help to address the abnormalities listed above.
Fibromyalgia and Thiamine Processing
There are several biochemical findings in FMS which are similar to those seen in thiamine deficiency, and a few lines of research indicate that there may be a problem with thiamine processing or utilization at the cellular level. Firstly, elevated whole blood pyruvate levels have been found in FMS, along with a greatly increased pyruvate/lactate ratio similar to that reported previously in thiamine deficiency. This same study also found reduced serum levels of the active form of thiamine – thiamine pyrophosphate (TPP). Secondly, Two thiamine-dependent enzymes (white cell pyruvate dehydrogenase and erythrocyte transketolase) had a much lower affinity for their coenzyme (TPP) in FMS patients. A lower affinity for the coenzyme means that higher levels of TPP are required to achieve normal enzyme activity. This is suggestive of a functional defect in thiamine utilization. Thirdly, another study showed a significantly elevated TPP-effect for transketolase activity, which is an indication of functional intracellular thiamine deficiency. The author also references two previous studies where they found much greater results using active TPP injections (20 out of 21 patients) when compared with thiamine alone (5 out of 13 patients). Unfortunately, those studies were published in French and I cannot locate them online. Finally, a more recent paper looked at various markers related to thiamine in FMS, alcoholism, and myofascial pain syndrome. Consistent with the findings laid out above, researchers found elevated pyruvate, an increased pyruvate/lactate ratio, and decreased affinity of transketolase for its coenzyme. Once again, the authors concluded that the changes seen in FMS demonstrate a functional problem with thiamine processing inside cells.
Can Thiamine Be Used To Treat Fibromyalgia?
As we have seen above, FMS is characterized by a wide variety of physiological changes both within the central nervous system and in the peripheral tissues. Abnormal central pain processing mechanisms have been identified, dorsal root ganglia neuronal hyperexcitability along with peripheral cell mitochondrial dysfunction, oxidative stress, inflammation, neuropathy and neurogenic inflammation. Biochemical findings indicate functional problems with thiamine metabolism, including lower levels of active thiamine, possible structural enzyme defects and reduced affinity for coenzymes, along with signs of functional deficiencies.
Many in the fibromyalgia community are likely familiar with the one study which used ultra-high doses of thiamine HCL to treat this condition. It was conducted by Dr. Constantini and coworkers at their lab based in Italy. Although this study only included a small sample size of three patients, it provided fascinating results which certainly merit further investigation.
The patients were administered daily doses of thiamine HCL ranged between 600mg-1800mg orally. After 20 days, they saw a 37%-71% reduction in fatigue and 50-80% reduction in pain. Two patients witnessed little to no benefit at lower doses, whereas they saw an abrupt improvement upon reaching the 1500-1800mg mark. This led the authors to theorize that the high doses might be necessary to bypass any potential intracellular transport defects or enzymatic abnormalities.
This study was the first of its kind that I know of to use mega-doses specifically for FMS. I have personally witnessed many people with this condition improve greatly with high dose thiamine. It is unfortunate that no other studies have been done to elucidate the mechanisms of action. These results certainly leave one wondering, how did thiamine provide such good results for these patients? Based on the established data of the pathophysiology of FMS and the mechanisms outlined above, the next section will attempt to explain why and how thiamine can improve the pain, fatigue, and other debilitating symptoms of this condition.
Thiamine For Fibromyalgia: The Mechanisms
A wide body of evidence has demonstrated anti-nociceptive and analgesic properties of thiamine when used in ultra high doses. In short, thiamine can work on both central and peripheral systems to reduce neuronal excitoxicity and hyperexcitability, inhibit glial cell activation and reduce inflammation, kickstart oxidative phosphorylation and improve mitochondrial function, and stimulate endogenous antioxidant systems. It has long been known that a lack of thiamine can produce severe disruptions in neurological function and inflict damage to several areas of the central nervous system. Of note, many of the structural and functional changes witnessed in thiamine deficiency closely resemble those in FMS.
Reduction of glutamate excitoxicity. Glutamate excitotoxicity is one phenomenon found in both FMS and thiamine deficiency. Evidence shows that thiamine deficiency increases extracellular glutamate concentrations to induce neurotoxic lesions in the brain. A deficiency also reduces glutamate uptake in neurons, which ordinarily helps to reduce extracellular glutamate concentrations, and this occurs likely through downregulation of GLT-1 and GLAST glutamate transporters. Through enhancing the activity of alpha-ketoglutarate dehydrogenase, a thiamine-dependent enzyme partially responsible for clearing excess glutamate, high-dose thiamine in animals has been shown to reduce glutamate concentrations and reduce oxidative stress.
Analgesic effects. Extremely high doses (250mg/kg) were shown to produce remarkable analgesic effects in a dose-dependent fashion in mice. The authors attributed these results to “an increased afferent inhibitory control of the spinal cord along with decreased response of thalamic neurons to nociceptive stimulation.” Several studies using electrophysiological equipment have shown that administration of B vitamins (thiamine , B6 and B12) can inhibit nociceptive neurons in the spinal dorsal horn and thalamus.
Tames hyperexcitable neurons. Recall that hyperexcitability of neurons in the dorsal root ganglia is also thought to FMS be one of the driving mechanisms behind sympathetic-mediated chronic pain in FMS. In vitro, thiamine administration reduces nerve hyperexcitability DRG neurons. High doses suppressed thermal hyperalgesia in animals and reduced hyperexcitability of DRG neurons by preventing alterations in sodium currents. These results suggest that high-dose thiamine may be acting to stabilize DRG neurons to reduce chronic pain. Furthermore, a combination of thiamine, riboflavin, and nicotinamide in very high doses prevented toxicity-induced nociception through reducing inflammatory cytokine (TNF-a & CXCL-1) production in dorsal root ganglia neurons and the thalamus.
Dampens neuroinflammation. Thiamine also appears to dampen neuroinflammatory responses in brain cells, which may help to explain its calming and analgesic effects in people with ongoing inflammatory issues. Two in vitro studies in (here and here ) demonstrated the ability of benfotiamine (a lipid-soluble thiamine derivative) to decrease pro-inflammatory cytokines, boost antioxidant responses to protect cell viability, and inactivate microglial cells in a model of neuroinflammation. High-dose thiamine has been shown to exert anti-inflammatory effects in numerous studies (here and here). The above findings showing thiamine’s protective role in the brain highlight the importance of using a form/derivative of this nutrient which can penetrate the blood brain barrier and saturate the central nervous system. Unlike benfotiamine, thiamine tetrahydrofurfuryl disulfide (TTFD) has the capacity to enter brain and increase brain thiamine content. When administered in high doses, thiamine and related derivatives have demonstrated significant anti-nociceptive effects in animal models of neuropathic and inflammatory pain (here, here and here). Human studies have also shown impressive analgesic effects, including patients with diabetic neuropathic pain (here and here).
Reduces neuropathy. Another way that thiamine may potentially help in cases of FMS relates to the type of neuropathy which has been identified in a large portion of these patients. If the allodynia and hyperalgesia is of neuropathic origin, then it makes perfect sense why thiamine can provide relief. Small fiber neuropathy commonly coexists with diabetes and is one of the primary forms of diabetic neuropathy. Both the central and peripheral nerves require large amounts of thiamine to maintain functionality, and one of the first signs of deficiency can relate to peripheral nerve complaints. Thiamine has long been studied for its role in neurological function, and thiamine derivatives have been shown on numerous occasions to improve diabetic neuropathy through reducing oxidative stress, improving redox status and nerve cell regeneration (here, here and here).
Corrects glutathione and reduces oxidative stress. Low affinity of transketolase for its coenzyme in FMS might help to explain to deficit in reduced glutathione and overall picture of oxidative stress. Transketolase is an enzyme which requires thiamine and magnesium, and is involved in the regeneration of glutathione through the pentose phosphate pathway. Low transketolase activity can be caused by genuine or functional thiamine deficiency, and high-dose thiamine can restore transketolase function. Furthermore, thiamine supplementation has been shown to protect cells from oxidative onslaught and improve reduced glutathione levels likely through its role as a transketolase cofactor.
Supports energy synthesis. In central and peripheral cells, mitochondrial dysfunction can be improved through the addition of nutrients which are required as cofactors in energy metabolism. As a cofactor and allosteric regulator of several enzymes, active thiamine possesses a great capacity to support mitochondrial energy synthesis.
Normalizes lactate. The buildup of muscle tissue lactate found in FMS and the elevated pyruvate can be attributed to a “metabolic block” or inactivation of the pyruvate dehydrogenase enzyme complex. Because thiamine is a key cofactor, inhibition or downregulation of this enzyme is one of the common findings in thiamine deficiency. High-dose thiamine has been used successfully in multiple studies to “kickstart” or increase the activity of this enzyme by a significant amount to normalize lactate and pyruvate concentrations and restore the cell’s ability to use oxygen. Tissue pH returns back to normal and metabolism is shifted back towards oxidative phosphorylation and away from glycolysis. Outside of the context of deficiency, this phenomenon is presumed to occur through inhibition of another enzyme called pyruvate dehydrogenase kinase – which essentially removes the “block” from the PDH complex. For this reason, high-dose thiamine possesses remarkable anti-tumor/anti-cancer properties also.
With the above in mind, is it any wonder why thiamine has been able to provide such benefits for people with FMS? Looking at the literature published on chronic pain, it seems that the powerful analgesic properties of thiamine have been utilized for a variety of disorders involving pain.
Thiamine Reduces Pain
One group of researchers investigated the analgesic effect thiamine in an animal model of pain induced by second-degree burns. They showed that local administration of 2-4mg was found to attenuate the pain caused by this injury. In another animal model of CFA-induced arthritis, high doses attenuate thermal hyperalgesia (pain), reduced TNF-a and IL-1B, and reduced paw edema which was an indicator of the inflammatory response. In children with chronic acrodynia (pain in the hands) and high pyruvate (similar to FMS), thiamine supplementation was shown to swiftly resolve symptoms. In combination with vitamin B6 and B12, thiamine has been used in cases of neuritis, PMS and painful vertebral syndrome.
If we reference back to much older research, the results are quite astonishing. It appears that the pain-relieving effects of thiamine have long been known – yet seemingly forgotten in the field of medical research. A paper published in the 1930s describes the efficacy of thiamine for the treatment of pain in amputation stomps. A daily injection of 10mg thiamine provided considerable pain relief in 26 of 30 cases. In 1940, researchers administered thiamine to patients presenting with painful varicose ulcers in the lower extremities. Of the 35 patients, 30 experienced relief from pain. Pain, heaviness, stiffness and pressure were relieved within 4-8 days after treatment, and when treatment was discontinued the symptoms returned in a milder form. The author also references another small trial in which 9 out of 10 patients experienced significant pain relief, and 8 experienced a complete resolution in symptoms. In that trial, the onset of symptom relief varied from 3 to 11 days. Another paper from 1941 demonstrated pain relieving benefits of thiamine in the field of dentistry. Intramuscular injections at the time of dental extraction were shown to prevent dry sockets, and those who developed dry sockets experienced pain relief when compared with controls. One more case describes a case of persistent bilateral shoulder joint pains cured with thiamine treatment.
Intraspinal injections were investigated in the late 1930s for relief from intractable pain and inflammatory/degenerative nervous system diseases. A total of 28 patients with various nervous system/pain disorder received treatment of between 10-100mg thiamine. According to the author:
After intraspinal injection of vitamin B1, improvement in varying degrees was noted in all cases. All felt better and looked better; appetites were increased, pain was lessened or abolished completely, muscular control improved, speech and gait improved, joints became looser, libido was increased, diplopia corrected. Some of the patients felt rejuvenated.
Interestingly, the author described a reaction similar to the “paradoxical reaction”, where some patients experienced a temporary worsening of symptoms including a slight elevation of temperature, weakness, stiffness of muscles and fingers, loss of appetite, buzzing or blowing in ears, and conjunctivitis lasting from several hours to several days. This was often followed by signs of improvement.
Much to my surprise, thiamine was apparently used as an analgesic and labor-inducer during childbirth in the Soviet Union and also in the West. A review published in 1951 found that a dose between 40-300mg produced some relief from pain in 50% of 622 patients. In 237 of these patients, 90% experienced shorter duration of labor. The authors also described their own research, where 35% experienced pain relief.
Relatively speaking, the therapeutic potential of this nutrient is practically unknown. I have personally witnessed immense improvements in several clients with FMS using this nutrient in high doses in conjunction with the necessary nutrient cofactors. I hope that you can now appreciate the potential benefits of thiamine for improving the symptoms of fibromyalgia and have a better understanding of the potential mechanisms behind how this nutrient works.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on Objective Nutrients on June 17, 2020 and republished here with permission on January 2021.
Image by Josh Clifford from Pixabay.