I could tell you that if a drug has a black-box warning stating that it can cause tendon ruptures, you shouldn’t take it if you are an athlete—after all, tendons are necessary for movement. Or, I could tell you about how the black-box warnings on fluoroquinolone antibiotics (Cipro, Levaquin, Avelox, Floxin, and their generic equivalents) are completely and utterly inadequate because fluoroquinolones not only lead to achilles tendon ruptures in those over 60, they lead to “a wide spectrum of musculoskeletal complications that involve not only tendon but also cartilage, bone, and muscle” in people of all ages.
I could describe the mechanisms through which fluoroquinolone antibiotics age cells and make people feel as if they are geriatric when they are young or middle-aged. No one wants to age prematurely, but athletes in particular want to keep their bodies youthful and strong.
I could tell you about the debilitating, chronic pain that people going through fluoroquinolone toxicity experience, or I could tell you about the autonomic nervous system dysfunction. Or, I could tell you about how fluoroquinolones downgrade GABA neurotransmitters and can lead to chronic insomnia and anxiety. All people, athletes included, want to avoid debilitating pain, autonomic nervous system dysfunction (and all of its manifestations), insomnia, and anxiety.
But technical information about the dangers of fluoroquinolone antibiotics isn’t near as convincing as true stories about the pain that fluoroquinolones have caused. Data in a study isn’t relatable, and neither are descriptions of mechanisms of action. However, people can relate to examples and case-studies, and I hope that athletes reading this will realize that fluoroquinolone antibiotics can hurt and disable all people, including athletes. Unless there is no alternative and one must take a fluoroquinolone to save his or her life, these drugs are too dangerous for athletes to use.
Jeremy’s Story
In a comment on a Consumer Reports article, “Fluoroquinolones Are Too Risky for Common Infections,” Jeremy stated:
“I took one dose of Levaquin 2.5 years ago and it ruined my life. I was/am an athlete and was administered it for a sinus issue. I was on crutches for 8 months and I am still in pain 24/7 with peripheral neuropathy. I can’t sleep and there is no respite from the pain. Please don’t take these drugs unless it’s a last resort… life and death. It’s not worth the pain and suffering, I didn’t know if I was going to make it for a long long time and may never recover or be able to kite surf, ski, back country, hike, backpack or even go up stairs easily again, ever!”
Athletic pursuits were a huge part of Jeremy’s life before he took Levaquin. Now he is in constant pain and fears that he will never again be able to do the sports and activities that he loves.
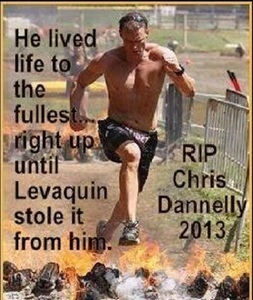
Chris Danelly’s Story
The picture of Chris Dannelly above speaks volumes. Chris was at the prime of his life and the peak of his fitness when he took levofloxacin. Tragically, after just two pills of levofloxacin, Chris suffered a toxic reaction (rhabdomyolysis) that took his life. He was not only an athlete, he was a loving husband and a father to two young children.
In this video Chris’s widow Kathy speaks out about Chris’s tragic death:
JMR’s Story
JMR was a 50 year old active and athletic woman before she took Ciprofloxacin. In the article, “Fluoroquinolone Antibiotics and Thyroid Problems: Is there a Connection?” she states:
“I remember the day of March 19, 2010 very well. That was the last day I ever went jogging. That was the last day I could have hopped on my bike and ridden 50 miles if I wanted to. That was the last day I ate my favorite breakfast of a 3-egg omelet topped with cheese and veggies, with 3 pieces of whole wheat toast slathered in butter and jam, 3 pancakes on the side, and at least a quart of milk. That was the last day I worked in my profession, brought home a paycheck, and was self sufficient financially. It was the day before I started taking Ciprofloxacin, a fluoroquinolone (FQ) antibiotic, for a simple UTI. And it was the last day I was a normal person with a normal life.”
Additionally, in “Adverse Drug Reactions (ADRs): We’re ALL at Risk” JMR describes the severity of her adverse reaction to ciprofloxacin:
“I’m lying in my bed, with my arms and legs straight out. I figured out pretty fast that any stress whatsoever on the tendons, makes things worse for days, weeks even. “Stress” includes not only trying to walk or use my arms or legs for any reason at all, but also simply bending my arms, or my knees, or my fingers, in one position for too long. What’s “too long”? Maybe 3-5 minutes or so. I can’t use crutches or a wheelchair, because both of those involve use of my arms and shoulders and hands, which are also out of commission. I can’t type or use the computer, because every tendon in my fingers, hands, wrists, and arms are affected and severely painful. I can’t hold up a book to read, because the weight of the book is too much and I can’t bend my arms, without increasing the tendon pain. The weight of the sheets on my toes causes severe pain in the tendons there. There must be tendons around the eye muscles too, because it hurts simply to move my eyes. So I lay there in my bed, with my arms and legs flat out, with my head still and my eyes closed, waiting. Waiting for what, I’m not sure. It’s hard to believe that I went jogging and bike riding and swimming only a few days ago. I’m also in shock. How in the world could a simple antibiotic that I took for a simple UTI do this to me?”
More information about the effects of ciprofloxacin on JMR’s life can be found on www.fluoroquinolonethyroid.com.
Terry’s Story
I don’t have a direct quote from Terry to illustrate her situation, so I’ll just do my best to summarize it. Terry loves tennis and plays it often. She’s not a professional tennis player by any means, but it is one of her favorite activities.
Terry took ciprofloxacin to treat a urinary tract infection. Three weeks later she returned to playing tennis and noticed that her ankles hurt after playing an easy game. She played tennis again a few days later and noticed that her ankles hurt worse than before, and that her wrists were starting to hurt. After a few months she went to her doctor and her doctor told her that she had multiple tears in her ankle tendons. Her knees became tender shortly thereafter. Now, with her ankles, wrists and knees in pain, the joy of playing tennis has been taken away from her. She is hopeful that her tendons will heal and that she will be able to play tennis like she did before she took ciprofloxacin, but she is scared that her tendons may continue to tear and rupture. Only time will tell.
Other Case Studies
The article, “Fluoroquinolone-induced serious, persistent, multisymptom adverse effects” published in the British Journal of Medicine, goes over four cases of people who were healthy, active and athletic prior to taking fluoroquinolone antibiotics who are now disabled because of their reactions. I recommend that everyone read through it prior to taking a fluoroquinolone antibiotic.
Mayo Clinic Physician Recommendations
In the article “Musculoskeletal Complications of Fluoroquinolones: Guidelines and Precautions for Usage in the Athletic Population” published by the American Academy of Physical Medicine and Rehabilitation, and written by three physicians with ties to the Mayo Clinic College of Medicine in Rochester, Minnesota, proposes the following guidelines for fluoroquinolone use in athletes:
- Athletes should avoid all use of fluoroquinolone antibiotics unless no alternative is available.
- Should a fluoroquinolone antibiotic be prescribed, the athlete, and ideally the coaching and athletic training staff, should be made aware of the increased risk for the development of musculoskeletal complications. Health Insurance Portability and Accountability Act guidelines should always be followed when discussing the athlete’s health with coaching and athletic training staff.
- Oral or injectable corticosteroids should not be administered concomitantly with fluoroquinolones.
- Consideration should be given to supplementation with magnesium and/or antioxidants during the fluoroquinolone treatment course if no contraindications are present.
- Training alterations should begin at the time of the first dose, including a reduction in high-intensity and ballistic activities and total training volume. The reductions should remain throughout the duration of the antibiotic course. If the athlete has no symptoms after completing the full course of the antibiotic, then a graduated return to full activity under direct medical supervision should be initiated, with close monitoring for the development of musculoskeletal symptoms.
- All athletic activity should cease at the onset of symptoms, with graduated return to activities when the person is asymptomatic. The fluoroquinolone should be discontinued if possible, and alternative antibiotic treatment should be prescribed if clinically indicated.
- Close monitoring should continue for [at least] one month from completion of the antibiotic course. The athlete should understand that symptoms have been reported as late as 6 months after fluoroquinolone exposure, and prompt medical evaluation should be sought if symptoms develop. During this period, special consideration should be given to adequate recovery between bouts of high-intensity activity or competitions.
Avoid Fluoroquinolones
Athletes, and everyone who values their tendons, muscles, cartilage, autonomic nervous system, central nervous system, and peripheral nerves, should avoid fluoroquinolone antibiotics whenever possible. Fluoroquinolones are powerful drugs with life-altering consequences. Adverse-reactions to fluoroquinolones are often severe. The people mentioned above certainly didn’t think that they could experience a life-altering adverse-reaction to an antibiotic, but it happened to them. Please heed their warnings and don’t let it happen to you.
Information about Fluoroquinolone Toxicity
Information about the author, and adverse reactions to fluoroquinolone antibiotics (Cipro/ciprofloxacin, Levaquin/levofloxacin, Avelox/moxifloxacin and Floxin/ofloxacin) can be found on Lisa Bloomquist’s site,www.floxiehope.com.
This article was first published on Hormone Matter in March 2016.