My issues began after the birth of my second child 21 years ago. I would get extreme indigestion for a couple days each month and my skin broke out. This continued for years until I ended up having several rounds of antibiotics. Months later, I developed severe and never ending acid reflux. After struggling for a year, my local health food store owner mentioned the blood type diet and recommended I avoid dairy. The result was magic. Unfortunately, this started a cascade of elimination diets that would set the tone for the next fifteen years.
After eliminating dairy and seeing a resolution of symptoms, at least temporarily, I decided to eliminate gluten too. As with the dairy, the indigestion disappeared temporarily when I eliminated gluten, but other symptoms eventually crept in, including hypothyroidism and bile reflux. I read about a vegetarian diet and decided to give it a try. Again amazing results from removing meat. The bile reflux disappeared. I thought things were going pretty well, but in these years I started to have other issues: ataxia, fatigue, heat intolerance, numbness and tingling, gait and bladder issues. In addition, I was always starving. I ate a tremendous amount of food each day, but at the same time I was losing weight.
My naturopath had mentioned possible problems with my gallbladder, but I didn’t think too much about it until I had constant pain. It was eventually discovered that I had a non-functioning gallbladder and I reluctantly had it removed, hoping it would solve my problems. I had tried changing my diet to the autoimmune paleo several times, but would always crash after a couple weeks. After surgery, I could eat meat without major issues, but nothing seemed to digest well. I felt like I never really recovered and other issues started to creep in.
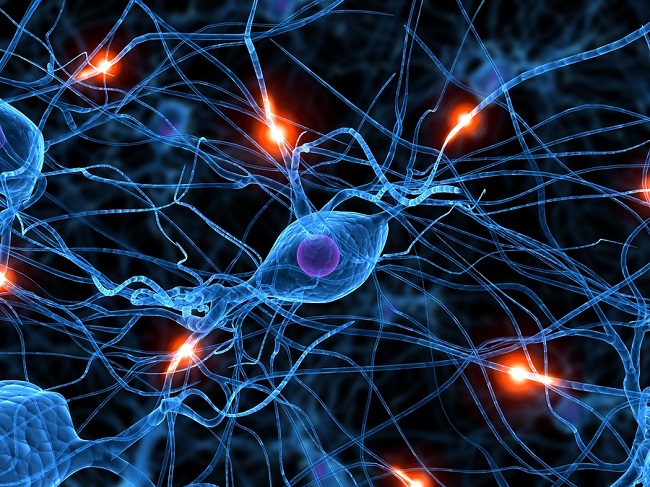
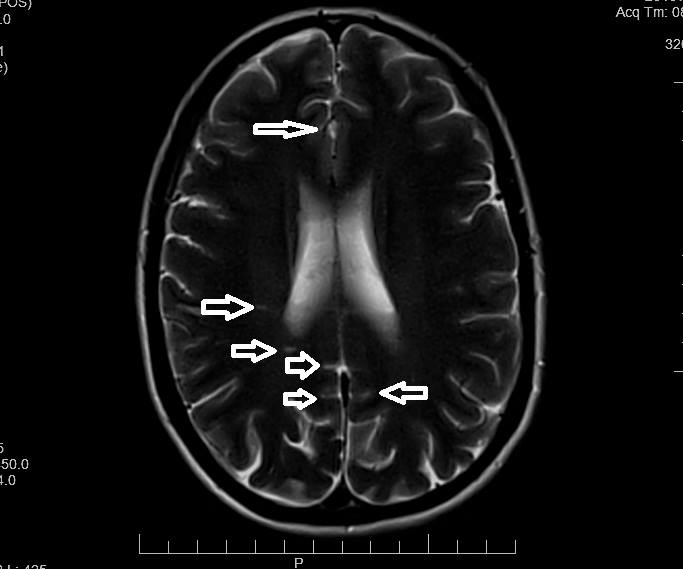
My calf muscles would spasm upon standing and I was so weak I was having difficulty walking a block. A year after surgery, I was diagnosed with primary progressive multiple sclerosis, as it matched my symptoms and lesions were seen on my cerebellum and down my spine. The hallmark of PPMS is neurodegeneration without inflammation. The next three and a half years were a quick decline. I quickly became unable to walk unaided, mainly because I was too fatigued and my muscles too weak. PPMS used to be called creeping paralysis and that is exactly what was happening; I was unable to move my arms or legs, my equilibrium was so off that I couldn’t stand without tipping over and I couldn’t look down to even zip up my jacket.
I had really bad edema in my lower legs and feet and they were a nice shade of purple. My brain was easily overwhelmed and not committing things to memory, which left me going in circles. I lost my appetite, but blamed it on my ever changing diet and my fear of eating the wrong food. I would alternate between diets, cutting various food groups with very limited success.
I visited multiple naturopaths, a functional medical doctor, a NUCCA chiropractor and a MS specialist. I have researched endlessly and have a cupboard full of supplements. I had tried B vitamins before but had not noticed a difference. I joined a Facebook group called Understanding Mitochondrial Nutrients and did not think much about the vitamin I needed most, thiamine, until a post by a desperate husband came up in my feed. I began to research thiamine and found I was able to piece together a timeline of my life based on a progressing thiamine deficiency. I am only three weeks into dosing with thiamine (I take 200mg thiamine HCL and 240mg benfotiamine) and a B complex, but it has made such a difference in my balance, fatigue, edema and mental energy. My appetite is back and I can zip up my coat! I am cautiously optimistic, only because I have suffered so much disappointment in the past. I am hopeful that I can make a recovery.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Thought Catalog on Unsplash.