The untimely death of 23-year-old Sasha McHale, daughter of professional basketball’s Hall of Famer Kevin McHale, recently shocked the world.
Sasha inherited her father’s athleticism, energy, enthusiasm for life, and love of the northern U.S. state of Minnesota. An insidious disease called lupus prematurely snatched Sasha from her family, friends, and life.
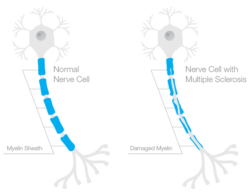
Lupus is a chronic autoimmune disease that attacks the body’s cells, tissues, and organs, and results in severe inflammation, fatigue, and, in some cases, death. The medical name for the most common form of the lupus is “systemic lupus erythematosus” (SLE). According to the Lupus Foundation of America, about 1.5 million Americans, and over five million people globally, suffer from a form of lupus. Ninety percent of persons diagnosed with the disease are women, many of whom are in their child-bearing years.
Mounting evidence suggests adequate vitamin D3 in the body may protect against the development of autoimmune diseases including lupus. Genetic and environmental factors including vitamin D3 deficiency have been linked to lupus. Sensitivity to sunlight, the primary source of vitamin D3, is common among SLE patients. Scientific research indicates a high prevalence of vitamin D3 deficiency among people suffering SLE:
Researchers at the University of Toronto Lupus Clinic studied 124 female SLE patients to understand, inter alia, their circulating vitamin D3 levels. Eighty-four percent of the women had vitamin D3 blood serum levels less than a sub-optimal reading of 32 ng/mL.
The Medical University of South Carolina conducted a study of vitamin D3 blood serum levels of 123 individuals who had been recently diagnosed with SLE. The findings suggested vitamin D3 deficiency as a possible risk factor for SLE.
Researchers studied 25 Canadian women diagnosed with SLE and found that over half of these patients had less than 20 ng/mL of vitamin D3 circulating in their blood. The research also suggested that hydroxychloroquine (HCQ), a drug used to treat SLE, may inhibit vitamin D3 production.
A study published in a 2012 edition of the journal Dermato-Endocrinology not only documented the prevalence of low vitamin D3 in SLE patients but recommended oral vitamin D3 supplementation for SLE patients. The researchers lauded the safety, low cost, and wide availability of vitamin D3 supplements as well as their potential effectiveness against SLE progression.
Maintaining adequate vitamin D3 levels may forestall the development of autoimmune diseases including lupus. In addition, vitamin D3’s capability to reduce inflammation may alleviate lupus symptoms. Further research is required to confirm the extent of vitamin D3’s connection with lupus.
Copyright ©2012 by Susan Rex Ryan
All rights reserved.