After many months of intense research, I firmly believe the birth control pill stinks, but who am I to say? I’m not an M.D. or a PhD. Even worse, I’m not a woman.
At the risk of being counter-cultural, I’d like to be completely transparent. I’m a bald, middle-aged, Catholic, white man from Texas. Clearly, I’m not allowed to have an opinion on The Pill, but I do. And, I’m passionate about it!
Now that I’ve given you every label you could possibly need to dismiss what I’m about to share, I plead with you to hear me out. My passion for this subject is not driven by a moral or political agenda. I have no deep-seated desire to tell women what they should or shouldn’t do. In fact, I have only one agenda – to expose the very real dangers of hormonal contraceptives.
I’m telling you who I am up front because we live in a culture of extremes. We’ve lost the art of moderation. It seems we are all either Conservative or Liberal; Pro- or Anti-; Us or Them… Defined by extremes, there is no middle ground. Regardless of which side we’re on, when someone offers a different perspective, we assume they are ‘one of them.’
I never dreamed I would be a women’s health activist, but that’s what I’ve become. I’m not even sure that label can stick to me, but I’m eager to wear it, even if I have to clip it on with safety pins.
My Distaste for The Pill
My distaste for The Pill predated any religion or spirituality in my life. For that matter, it also predated being bald, middle-aged, and Texan.
My wife and I were young and deeply in love. Somehow, that fact came up in a discussion with her doctor. She had gone in with allergies, but came out with The Pill. That was fine by us. We hated condoms, and this sounded like the perfect solution. The doctor didn’t mention any side effects, and since it had been on the market for decades, she never thought to question its safety.
On about the fourth month, a little pamphlet fell out as she opened the package. I picked it up, and started reading. I was horrified. “Honey, did the doctor mention any of these side effects to you?”
“What side effects?”
We sifted through the complicated text, and discussed some of the warnings — breast and cervical cancer, strokes, and heart disease. They were especially disconcerting given her family history. She asked whether the doctor would have given it to her if he thought it was dangerous.
Ultimately, it was a long, thoughtful conversation that ended with me saying, “I can’t tell you what to do, but for me, if taking this pill means I get to spend even one less day with you at the end of our lives, it’s not worth it.”
It surprised me how much relief that statement brought her. The pills had apparently been making her feel crazy, and she decided to stop taking them immediately. Beyond my wife, my attitude about The Pill was indifferent. I never thought to ask my sisters if they had read the pamphlet, or if their doctors had warned them. It didn’t seem like my place.
Was it my place? Am I even allowed to talk about that with women beyond my wife? Where do my rights and responsibilities end?
Years passed. Then, a series of events brought me in contact with information that left me a little smarter than the average bear… at least where The Pill is concerned. When you’re privy to information that you know most women haven’t been told about The Pill, does your responsibility change? I think it does. I have sisters and nieces who suffered consequences because I didn’t discuss The Pill with them sooner. I believe anyone who learns the truth about The Pill should act on the urge to shout the news, and drown out the silence of the doctors.
My Focus on The Pill
As a writer and media producer, it was work that first inspired my pill quest. Writing requires a natural curiosity. Whether I’m developing a documentary or creating a marketing piece for a corporate client, I’m always looking for an interesting story.
A medical project early last year brought me in contact with one of the world’s leading authorities on a certain disease (I will be more specific about the disease in future posts). I sat in on a meeting as this revered doctor spoke to a group of young specialists about the basics of the disease.
He said, “We’ve known from the beginning that estrogen plays a key role… because 75- to 80-percent of diagnoses are women, and we know the role estrogen plays in a woman’s immune system.” He explained how environmental estrogens get into our system, and mimic natural estrogen.
My ‘interesting story’ radar went off even though it had nothing to do with the project at hand. I pulled out my phone. A quick Google search revealed that the incidence of this disease began climbing rapidly in the early 70’s.
I benefited from limited knowledge. All I knew of the disease was a time frame, and what triggered it – chemicals mimicking natural estrogen. The only example I could think of was birth control pills. Based on what the good doctor had said, I assumed the connection must be well known in the medical community, but was surprised I had never heard about it.
I struck up a conversation with him after the meeting, and asked exactly what role The Pill had played in all of this. He replied, “None at all.”
I was dumbfounded. “That seems impossible.” I wasn’t doubting him. In fact, I completely believed him, regardless how impossible it seemed. After all, he was the world-renowned authority.
He doubled down, “There hasn’t been any evidence linking The Pill to [the disease].”
The conversation continued for a while, but didn’t advance. It concluded with him saying, “Certainly, there are more questions than answers. And more research needs to be done.”
I walked away feeling confused – as if he had waved his hand and said, “These aren’t the droids you’re looking for.”
That Nagging Feeling
I was still thinking about the encounter when I got back to my hotel room that evening. I pulled out my computer and did a search for the disease, plus “oral contraceptives.” Among the top results was an article about a new study that found women who take The Pill are 50% more likely to have this disease than nonusers.
I wondered whether the doctor had been unaware of this study. The question didn’t linger long. He was quoted halfway through the article. In black-and-white, the world-renowned authority told women they shouldn’t stop taking The Pill because of this study, and that they needed to weigh the benefits against a very small increased risk of developing the disease.
Had he lied to me? At best, he had certainly obfuscated the facts. Maybe he just thought it would be too deep for a simpleton, and it was easier to say that no connection existed.
During the next few weeks, I continued my search, and found several studies over the past 50 years that had linked The Pill to this disease. And for each study, it seemed there were always leading authorities who were eager to say the benefits still outweighed the risks. This was a pattern I observed frequently as I broadened my search to include other ailments.
Questions About The Pill
Those early searches left me with two burning questions that drove me to dig deeper:
- Are doctors being forthright with women about hormonal contraceptives so that they can make truly informed decisions?
- Why is the medical community always eager to downplay studies that find risks associated with birth control pills?
Answers to the second question tend to dance around the political landscape. So, for the purposes of my posts on Hormones Matter, I will focus more on the answers to the first question. However, I do think it’s important to lay a little more foundation to explain how I formed my opinions.
In my next post, I will tell you how a feminist, a crusty old reporter, and a 102-year old man fueled my continued interest.

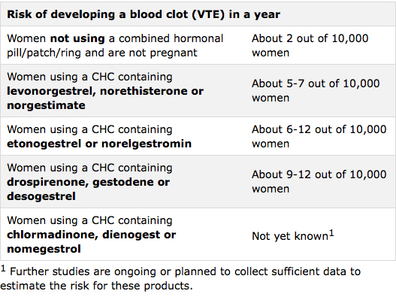
The FDA approved The Pill despite it not being proven safe. Today, it has been linked to everything from blood clots and cancer to lupus and Crohn’s disease — and still has not been proven safe.
This book explores the medical and historical disconnects that brought us to this point.
Last updated on October 21, 2023 at 9:38 pm – Image source: Amazon Affiliate Program. All statements without guarantee.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.