Although hypertension has become almost exclusively used to indicate high blood pressure, it is worth examining the true underlying meaning. The prefix “hyper” is from the Greek, meaning over or above. Tension is defined as “the state of being stretched tight”. Perhaps then it is worth looking at how this applies to blood pressure.
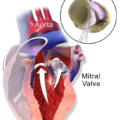
When a blood pressure is measured, there are always two figures represented. The higher number is known as “systolic” and the lower one as “diastolic”. The systolic is when the heart is contracting and indicates the ability of the arterial system to expand enough to accommodate the pressure from an increased volume of blood. The diastolic indicates the pressure in the arterial system when the heart is resting between beats. We are therefore looking at the highest and lowest pressures in a closed tube system that must be capable of expanding and contracting.
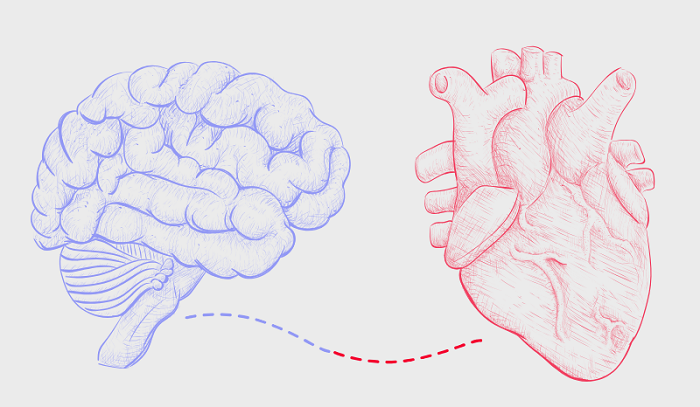
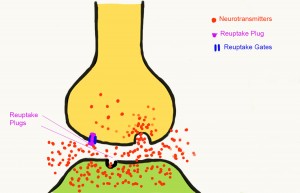
Since the system is made from live cells, it does not behave like a rubber tube with elastic recoil. The arteries where blood pressure is measured are lined with muscles. It is the contraction and relaxation of these muscles that control the capacity of the artery to accommodate the amount of blood arriving from the heart. The muscles are controlled by nerves carrying messages from the brain. These muscles are completely different from those that are activated willingly, such as those in the limbs. They are contracted and relaxed automatically by a part of the brain that acts more like a computer. The body muscles are activated by a nervous system known as “voluntary”. The arterial muscles are activated by a completely separate an involuntary nervous system known as autonomic (ANS). We therefore have to examine the control mechanisms.
Understanding the Autonomic Nervous System
I have discussed this nervous system many times in Hormones Matter because, when it goes wrong, it is a potent source of disease. The nerves of this system go to every organ within the body. The control system is in the lower part of the brain. It consists of two channels. One is known as sympathetic: the other is known as parasympathetic. Although they work together, their actions oppose each other and I will try briefly to outline this dichotomy.
Sympathetic. The sympathetic nervous system is designed for both physical and mental action through a reflex mechanism known as the fight-or-flight. It prepares us to meet an enemy or escape from danger. One of its actions is to raise the blood pressure. It does this by contracting the arterial muscles already described.
Parasympathetic. When the action is completed, the brain controls automatically withdraw the activity of the sympathetic and initiate those of the parasympathetic nervous system. When this happens, the body is prepared for resting.
Chronic Activation of the Sympathetic Nervous System
There is a large amount of evidence in the medical literature that this is the primary cause of chronically high blood pressure. If the system is healthy, the blood pressure will go down on completion of the action. If not, the blood pressure remains elevated. From here, I am going to hypothesize why this happens. Please remember as you read it that it is a hypothesis, not a proven fact.
Hypoxia. This word simply means lack of oxygen. Obviously, this is a dangerous state for the brain and it is not surprising that it will activate the sympathetic component described above, including raising the blood pressure.
Pseudo-hypoxia. The prefix “pseudo”, meaning false, or sham (from the Greek, lying, false) has been used in the medical literature to describe a state that is exactly like that of hypoxia when the presence of oxygen is normal. In order to understand this, focus on the fact that oxygen must be introduced to the body but is completely useless unless it is consumed. Therefore we must try to indicate how oxygen consumption occurs.
Oxidation and burning. All forms of burning are derived from oxygen combining with a fuel, liberating heat energy. That is why we are warm blooded, but other forms of energy are produced to drive physical and mental function. Because the burning is incomplete, ash is formed. Our cells derive their energy by the oxygen, delivered in the blood from the lung, combining with glucose. The “ash” is carbon dioxide and water, discarded in the breath. The oxidation of glucose is governed by a set of enzymes that require the vitamin B complex for their action. The leader of this orchestration appears to be vitamin B1 (thiamine). That is why many papers have appeared in the medical literature that describes thiamine deficiency as a cause of pseudo-hypoxia. Its function is to catalyze the enzymes essential for oxidation. Its deficiency results in lack of sufficient energy. It is therefore not surprising that one of the symptoms of thiamine deficiency is fatigue.
Calorie/thiamine ratio. A healthy diet provides us with calorie producing elements that are broken down to glucose and used as fuel. The amount of thiamine provides a normal calorie/thiamine ratio that enables efficient oxidation. If we load the diet with empty calories (calories without essential non-calorie nutrients that include thiamine) the calorie/thiamine ratio becomes abnormal. Measuring the concentration of thiamine in the blood would be normal for a healthy diet but inadequate to meet the demand of the empty calorie load. The laboratory method for identifying thiamine deficiency is by measuring it in the blood. If the result is reported by the laboratory as normal, the relevant symptoms produced by inadequate oxidation may well be ascribed to causes other than thiamine deficiency.
Hypothesis: High Calorie Malnutrition Induces Chronic Sympathetic Overdrive
I suspect that a common cause of hypertension is high calorie malnutrition, inducing a state of chronic sympathetic overdrive. It may be why obesity in children often foretells their rise in blood pressure. Perhaps another cause is the gradual diminution of oxidation associated with aging. There are genetic mechanisms that are turned on by hypoxia and these also may be activated by pseudo-hypoxia, e.g. thiamine deficiency.
Spontaneously Hypertensive Rats
Lipothiamin is a synthetic derivative of thiamine. Its biologic properties enable it to be used as a drug. A rat known as SHR (spontaneously hypertensive rat) is used as the animal model for studying the effect of antihypertensive drugs. Many years ago I took a group of these rats and treated them with Lipothiamin to see if it would prevent the rise in blood pressure that always occurs in these animals. There was a statistically significant difference between the experimental rats and the controls, indicating that this thiamine derivative did indeed prevent the spontaneous rise in blood pressure. This experiment is published in our book (Lonsdale D, Marrs C. Thiamine Deficiency Disease, Dysautonomia and High Calorie Malnutrition). It obviously requires human subjects to research the use of this completely non-toxic, nutrient/drug derivative but nevertheless provides us with solid clues about hypertension.
Conclusion: Diet Matters
It has been said that simplicity must be distilled out of complexity in order to make complex issues usable. The brain/body, whether we like to recognize it or not, is an “electrochemical machine” that must obey all the physical laws designed by Mother Nature. Health is governed by only three factors:
- Genetics: the enormous complexity is dictated by a code written in DNA. Passage from generation to generation makes mistakes and represents our inheritance.
- Stress: defined as anything that requires physical/mental defensive response. The response, designed for relatively short term action, demands a huge consumption of energy.
- Nutrition: this is the only one of the three issues that we can control. It must supply both fuel and the multiple factors that enable the fuel to be turned into energy.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.