Numerous studies have shown a strong correlation between removal of both ovaries / bilateral oophorectomy (castration) and accelerated aging as measured by an increased risk of chronic health conditions. Hysterectomy / uterus removal with preservation of both ovaries is also associated with some of these chronic conditions. These include heart disease, stroke, metabolic syndrome, osteoporosis, hip fracture, lung cancer, colorectal cancer, dementia, Parkinsonism, impaired cognition and memory, mood disorders, sleep disorders, adverse skin and body composition changes, adverse ocular changes including glaucoma, impaired sexual function, more severe hot flushes and urogenital atrophy. Wow, that’s quite a list!
Ovaries: Health Powerhouses
This 2016 article titled “Study: Remove ovaries, age faster” sums up the findings of Mayo Clinic researchers proving yet again the harmful and unethical practice of ovary removal. The study found that ovary removal (oophorectomy) is associated with a higher incidence of 18 chronic conditions and should be discontinued in women who are not at high risk for ovarian cancer. Although this study cites the increase in chronic conditions in women who undergo oophorectomy before age 46, other studies have shown that oophorectomy even after menopause does more harm than good. Here is one that showed that to be true up to age 75.
The ovaries have both reproductive and endocrine functions as detailed in this International Menopause Society article. After menopause, the ovaries produce mostly androgens, some of which are converted into estrogen. Testosterone levels are more than 40% lower in women without ovaries compared to intact women. Women without their uterus likewise have lower levels but not as low as women without ovaries per this article. Estrogen therapy mitigates some but not all of the increased health risks of oophorectomy. But estrogen further reduces androgen levels increasing risk of osteoporosis and fracture. Nothing can replace the lifelong functions of the ovaries (and uterus).
The Uterus / Ovaries / Tubes Connection
The harms of ovary removal would also apply to ovarian failure that commonly occurs after hysterectomy and some other medical treatments. As previously cited, women who have had a hysterectomy have lower levels of testosterone. According to this 1986 publication, 39% of these women showed signs of ovarian failure. This study showed a nearly 2-fold increased risk of ovarian failure when both ovaries were preserved and nearly 3-fold when one was preserved. This likely explains the increased risk of heart disease and metabolic conditions as shown by multiple studies including this recent Mayo Clinic one. However, per this 1982 study, the uterus itself protects women from heart disease via the uterine substance prostacyclin. Loss of bone density is another harm of hysterectomy as shown by multiple studies such as this one.
Removal of even one ovary (unilateral oophorectomy) without hysterectomy is also harmful. Studies out of the Mayo Clinic showed increased risks of cognitive impairment or dementia and parkinsonism. Colorectal cancer is another increased risk according to this Chinese study and this Swedish one.
The Fallopian tubes appear to impair ovarian function to some degree as evidenced by Post Tubal Ligation / Sterilization Syndrome. This study shows an increase in Follicle Stimulating Hormone (FSH) after tube removal (salpingectomy).
Ovarian impairment after hysterectomy or salpingectomy is thought to be the mechanism of the reduced risk of ovarian cancer which is already rare.
The Uterus: Anatomy, Sex, Cancer Prevention
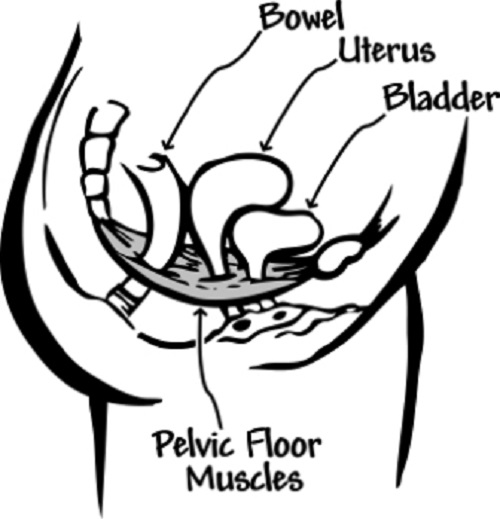
Hysterectomy is associated with other harms besides impaired ovarian / endocrine function. The uterus and its ligaments / pelvic support structures are essential for pelvic organ integrity as well as skeletal integrity. The effects on these structures and functions are detailed here and here. This article shows the many hysterectomized women lamenting their “broken bodies” – changes to their figures, back, hip and midsection pain, pelvic pain, bladder and bowel issues, and effects of severed nerves and blood vessels.
The uterus and associated nerves and blood vessels play a key role in sexuality and vibrancy. You can hear the desperation in women’s comments about the devastating sexual losses and feelings of emotional emptiness.
There is an increased risk of renal cell, thyroid, and colorectal cancers after hysterectomy. How ironic when cancer fear tactics are commonly used to market hysterectomy and/or oophorectomy.
Adhesions that commonly form after these surgeries can cause serious problems especially in the long term. Surgical complications – nerve injuries, bladder, bowel and ureter injuries, vaginal cuff dehiscence, a too short vagina, infections, hemorrhage – are more common than indicated by gynecologists.
Although “The Miraculous Uterus” article fails to mention the anatomical harms, it is otherwise “spot on.” It talks about the “ovarian conservation scam” and that “passion, love, ecstasy, the emotional essence that drives human achievement, forever after elude them.” This explains why “there’s no effective outrage against the barbarism of hysterectomy.”
Compelling Evidence of Harm
Clearly, there is compelling medical evidence that both hysterectomy and oophorectomy are destructive surgeries. Unfortunately, some hysterectomy forums censor negative posts giving a slanted view of the life shattering effects. Here is a sampling of women’s experiences on the Gyn Reform site.
The medical literature on the harms of these surgeries dates back over a century. Listed below are a small number of the numerous publications (minus the ovarian failure studies cited above). The Gyn Reform website has a fairly comprehensive list of resources on oophorectomy. Its Ovaries for Life sister site provides a good overview of the lifelong importance of our ovaries.
1912 – The Physiological Influence of Ovarian Secretion
1914 – Nervous and Mental Disturbances following Castration in Women
1958 – The controversial ovary
1973 – Osteoporosis after Oophorectomy for Non-malignant Disease in Premenopausal Women
“Oophorectomy before the age of 45 years was found to be associated with a significantly increased prevalence of osteoporosis within three to six years of operation.”
1978 – The emotional and psychosexual aspects of hysterectomy
1981 – Premenopausal hysterectomy and cardiovascular disease
1981 – Sexual response after hysterectomy-oophorectomy: Recent studies and reconsideration of psychogenesis
1981 – The role of estrogen and oophorectomy in immune synovitis
1982 – Prostacyclin from the uterus and woman’s cardiovascular advantage
1989 – The effects of simple hysterectomy on vesicourethral function
“The results show that simple hysterectomy is associated with a significant incidence of post-operative vesicourethral dysfunction and that there is an identifiable neurological abnormality incurred at operation which is pertinent to the subsequent disordered voiding.”
1990 – Effects of bilateral oophorectomy on lipoprotein metabolism
1994 – The climacteric ovary as a functional gonadotropin-driven androgen-producing gland
1996 – Urinary incontinence in older women: who is at risk? Study of Osteoporotic Fractures Research Group
“Urinary incontinence is a common problem in older women, more common than most chronic medical conditions. Of the associated factors that are preventable or modifiable, obesity and hysterectomy may have the greatest impact on the prevalence of daily incontinence.”
1997 – Bladder, bowel and sexual function after hysterectomy for benign conditions
1998 – Ovaries, androgens and the menopause: practical applications
1998 – Influence of bilateral oophorectomy upon lipid metabolism
1999 – Estrogen and movement disorders
2000 – The hypothalamic-pituitary-adrenal and gonadal axes in rheumatoid arthritis
2000 – Risk of myocardial infarction after oophorectomy and hysterectomy
2005 – Ovarian conservation at the time of hysterectomy for benign disease
“Ovarian conservation until age 65 benefits long-term survival…. There is sustained, but decreasing, benefit until the age of 75, when excess mortality for oophorectomy is less than 1%.”
2007 – Ovarian conservation at the time of hysterectomy for benign disease
“Approximately 78% of women between the ages of 45 and 64 years have prophylactic oophorectomy when hysterectomy is performed for benign disease…. Therefore, the decision to perform prophylactic oophorectomy should be approached with great caution for the majority of women who are at low risk of developing ovarian cancer.”
“In no analysis or age group was oophorectomy associated with increased survival.”
2010 – Current indications and role of surgery in the management of sigmoid diverticulitis
“A previous history of hysterectomy is a valuable clinical clue to the correct diagnosis as colovaginal and colovesical fistulas are rare in females with their uterus in place, as the uterus becomes a screen interposed between the inflamed colon and the bladder and vagina.”
2012 – Oophorectomy for whom and at what age? Primum non nocere
2016 – Study: Remove ovaries, age faster
2017 – Cardiovascular and metabolic morbidity after hysterectomy with ovarian conservation: a cohort study
A Harmful Practice That Won’t Die
Ovary removal / castration was introduced by Robert Battey in 1872 and “was practised widely for several decades….. Better insight into female physiology and ovarian function finally pushed the sinister operation of Robert Battey from the scene.” This publication refers to Battey’s operation as “barbaric.”
Despite the long-standing and compelling evidence of harm, these surgeries continue at alarming rates. Publications are misleading in that they report inpatient surgeries despite the large majority being outpatient (70% in 2014). This 2008 article reported that oophorectomies “more than doubled in frequency since the 1960’s.” According to results of a FOIA request by Ovaries for Life, there are over 700,000 oophorectomies every year despite there being only ~22,000 cases of ovarian cancer. Hysterectomy figures obtained by Ovaries for Life are also shocking at 830,000 in light of less than 70,000 cases of endometrial and cervical cancers.
Many media reports have questioned the high rate of these surgeries since gynecologic cancers are rare. The oldest one I could find was dated 1969. I found about three articles per decade in the mainstream media since then. According to the Athena Institute, half of U.S. medical schools in 1986 “had changed their suggestions and were now recommending a reconsideration of the common practice of ovariectomy.” Evidently, that never took hold.
Congress held two hearings on hysterectomy, one in 1976 and one in 1993. The 1993 transcripts state that the hysterectomy rate increased 250% in women ages 15 to 24 and 186% in ages 25 to 34 from 1965 to 1984! Despite these shocking statistics, it appears that no action was taken after either hearing.
According to this “Reassessing Hysterectomy” article, the Agency for Healthcare Research and Quality sponsored research and conferences on the overuse of hysterectomy in the 1990’s. This article is packed with information on the prevalence and harms of hysterectomy and oophorectomy as well as alternative treatment options. Yet, the high rate of hysterectomy has continued such that 45% of women will end up having one. Citing 2006 data, the oophorectomy rate was 73% of the hysterectomy rate.
How to End the Harm?
I’ve been researching this subject for over 10 years and sharing my experience and knowledge on various websites. It’s shocking how many women are misled and deceived into these surgeries. Age doesn’t seem to matter; younger and younger women are undergoing these surgeries. This appears to be the biggest surgical racket and women’s healthcare con as discussed here.
There are a number of issues that perpetuate the gross overuse of these harmful surgeries. These include:
- These surgeries and “forever after” care are very lucrative.
- The public has been led to believe that the female organs are disposable after childbearing is complete.
- Medical education and decades of practice have made these surgeries “a standard of care.”
- Informed consent is seriously lacking.
- Gynecology consent forms are open ended giving surgeons “carte blanche” to remove organs unnecessarily.
- We still live in a climate of gender disparity / male dominance.
As you can see from the list of publications above, some study authors have called out the practice of ovary removal as unethical. Numerous professional societies have issued guidelines discouraging its use in most women. But most have been silent on the overuse of hysterectomy despite its many harms.
Why has our government not stepped in to address this egregious harm? Women who have contacted their legislators have been met with indifference. Gyn Reform reported on their experiences with legislators and other authorities who can effect change. The non-profit HERS Foundation has been educating women and advocating for informed consent legislation since the 1980’s.
Why do insurance companies approve so many of these surgeries that are rarely necessary? Not only are the surgeries themselves expensive, treatments for the chronic after effects are costly. Reining in unnecessary treatments especially those that cause lifelong harm would go a long way towards making healthcare more affordable.
Why has Graduate Medical Education (GME) not changed their surgical requirements to favor organ preservation? Each resident must do at least 70 hysterectomies but there is no requirement for myomectomy (fibroid removal). Residents don’t need to do any cystectomies (cyst removals) either which is partly why so many women lose ovaries for benign ovarian cysts. Here are the GME ob/gyn requirements.
A popular mantra at Tufts in the 1970’s – “There’s no room in the tomb for the womb” – reflects this culture of the disposable uterus and gynecologists’ obsession with its removal. Insurance reimbursement rates are also to blame as they incentivize hysterectomy and oophorectomy over myomectomy and cystectomy. In many cases, medical management versus surgery is the appropriate course. The “Reassessing Hysterectomy” article cited above lists a number of treatment options for gynecologic problems. Revamping reimbursement rates to strongly favor organ preservation should eventually force GME to change their requirements. But how do we make that happen?
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Lucas Cranach the Elder, Public domain, via Wikimedia Commons