I have always preferred natural processes. I had four natural births using Lamaze technique. I breastfed. I was a registered nurse. I knew my ob-gyn doctors for years. I never expected my life to take a sharp and unnecessary turn for the worse, but it did, after I had, what was an essentially unneeded hysterectomy with oophorectomy.
A Total Hysterectomy for a Benign Ovarian Cyst
In 1990, I was 39 years old. I was physically active, I worked out daily. My blood pressure always in the 110/70 range. I scheduled my annual exam for mid March. My cycles were regular. I never had a suspicious pap smear. A couple years previously, however, I noticed some pain on ovulation. I asked the doctor if I might have endometriosis. She said she couldn’t find any evidence on exam.
My appointment was a shock. She found a mass near my right ovary. I was scheduled for an ultrasound. The ultrasound showed a 4cm mass.
I returned to the doctor with my husband. She said the mass was likely benign, but it should be removed. She asked if we planned any more children, we said no. She then recommended that I should have a total hysterectomy and my ovaries would also be removed (TAH-BSO). Her reason was that I might have future masses. She said I was in great shape, that I shouldn’t have any weight problems. She would do a Pfannenstiel incision (bikini cut) and it would fade to a small light scar. I was shocked, my mother was going through chemotherapy for cancer. What if I had another mass later that would be cancerous!
We scheduled surgery in two weeks. She gave us the ACOG hysterectomy brochure. I talked to a couple of friends that had the surgery. Not much to it, just rest a lot after surgery. They seemed fine, and hoped I would too. I called my doctor with a few questions, how will I feel after surgery and how might it effect sex. She said the Premarin would keep me feeling just as my natural estrogen has done.
Now the date was closing in, and my doubts were rising. I was busy with my four children, age 9 to 17. I read the ACOG brochure, it seemed too simple. The day before surgery, I asked my husband if we could go to the bookstore to see if we are missing something. He felt we had ample information from the doctor and friends, and yes, the ACOG brochure. We were both nervous. My husband didn’t want to lose me should I not have surgery. I was nervous about my future. My gut feeling was not to do it, but my brain told me that I don’t want a worse situation, if I don’t have the surgery. It haunts me to this day, I had that last chance to learn the truth and I did not take it.
A Total Abdominal Hysterectomy and Bilateral Salpingo Oophorectomy
The surgery was scheduled for April 5, 1990 at 1pm. I was terrified. My husband was so scared, he barely spoke to me. When I woke up in the recovery room, I felt a large dressing on my abdomen. I told the nurse “I just want to go home.” The doctor came in Saturday morning. She told me she found a lot of endometriosis. She detailed how much of it she cleared out. She said I would never have to deal with it again.
I went home Monday, I felt pretty good. I had a lot of abdominal swelling, nut that night I got up to go to the bathroom. It was then when I broke down and cried. Two weeks later, I took a good look at my abdomen and saw the horrible swelling over the incision. I showed it to my husband and he reminded me that it should take about six weeks to heal. He was very quiet and distant since the surgery.
I went to the doctor and she was startled when she saw my abdomen. She said it should be better in the coming months.
Learning the Truth
I was frustrated, I went to a bookstore to search what happened. I thought it was a hysterectomy issue. I found Hysterectomy: Before and After by Winnifred Cutler. As I glanced through the pages, it was a sharp contrast to the ACOG (sales) brochure. This was the information I needed BEFORE surgery! I began to tear up, I bought the book and went home. I could not understand why the doctor and ACOG would not inform women of these after effects. Now my abdomen problem was the least of my problems.
I asked my husband to read the book. He did but maintained the doctor gave us all the information we needed. I felt betrayed by everyone I had believed and trusted. No one had been honest with me. At that point, I was prescribed Prozac.
My post-op appointment was tense. I told the doctor that I had numbness in my right thigh, no response. I had insomnia, breast pain from the high dose of Premarin. There was no improvement with my abdomen. She told me “Just don’t look in the mirror”. By that time, my husband knew just how these doctors work. He had no doubt that the surgery was not necessary.
Hysterectomy Consequences
In March 1991, I went to another state and had a mini-abdominoplasty for scar revision. When the cosmetic surgeon saw the scar he said “That incision was closed unevenly!”. The three cosmetic surgeons in my area never hinted that my gynecologist was at fault. So, after my surgery I submitted my records from him with before and after photos. Anthem reimbursed me for the abdominoplasty.
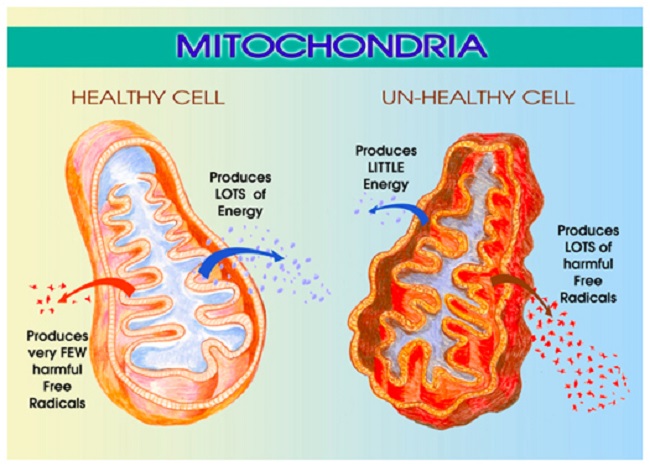
I felt better about my appearance, but the after effects of hysterectomy and ovary loss were beginning to pile up. I could not have the internal orgasms I had before. Still had insomnia, thigh numbness, and problems with Premarin. I wasn’t myself, I had anger and rage. I was tired, physically exhausted.
I was on Zoloft for a year and gained nearly 60 pounds. I finally ‘quit’ doctors. In 2001, I became a vegetarian. I lost most of my weight, but I still am 30 pounds over my ‘intact’ weight. I eventually could not wear contact lenses due to eye dryness. I still have episodes of rage and anger, panic attacks and on going depression. I have low libido, and few slight orgasms, along with bad back pain, knee pain, sciatica, and hip and joint pain.
I was 5’4 and now measure 5’2. I can only get one finger (normal is 2 to 3 fingers) between my ribs and pelvic bones due to post hysterectomy skeletal changes. In February 2017, I was diagnosed with bladder cancer. Fortunately, it was low grade and manageable. It bothers me to ‘need a doctor’. There are studies linking hysterectomy and ovary removal to both bladder cancer and renal cell carcinoma.
Where I Am Now
I am now 67. I still grieve my organ loss and the negative impact on my life. I am trapped in a body that is not mine. I recently looked at a picture of me at one year old. I wondered if that little girl would have known her life and happiness would end in 38 years.
- I could have gone to a bookstore to research the surgery the same day I scheduled it.
- I would have had a second, third or fourth opinion.
- I should have listened to my gut instinct.
Research, research and research. You can’t undo the damage! Don’t let the opinions of others cost you your well-being. You are the one that has to live with the consequences! They do not!
Share Your Hysterectomy Story
If you have a hysterectomy story, publish it here on Hormones Matter. Every story counts. Send us a note for more details.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by 412designs from Pixabay.
This story was published originally on May 16, 2018.