Everyone is aware of the proverb about the ostrich with its head in the sand. It has been a recurrent problem in medicine throughout its history. Louis Pasteur discovered that organisms, only visible with a microscope, caused disease. It became the first paradigm in medicine, accepted by all eventually. Pasteur spent eighty percent of his professional life in trying to get his ideas to stick. What would he have accomplished in addition to these discoveries if they had been readily accepted?
It is interesting to note, however, that on his deathbed he reportedly said “I was wrong: it is the defenses of the body that really matter”. Did he, in fact, provide us with a concept leading to a second paradigm in medicine – that maintaining host defenses matter as much as killing the pathogenic invaders? This post attempts to address this issue. What does it mean to bolster host defenses? Is this the next paradigm in medicine? And if it is, do physicians, like the mighty ostrich, have their heads in the sand when it comes to understanding host defenses?
The First Paradigm of Medicine: Kill the Enemy
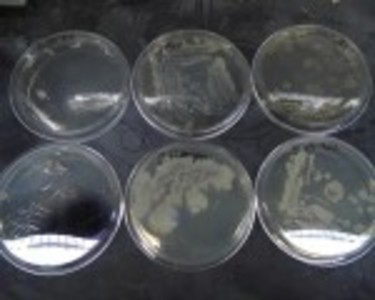
The discovery of microorganisms led naturally to the idea of killing them without killing the patient. After many frustrating years, during which many lives were undoubtedly sacrificed, the discovery of penicillin opened the antibiotic era. During its golden age, antibiotics have indeed saved many lives, but we all know that bacterial resistance is giving rise to new problems. As new antibiotics are discovered or synthesized, they have to become more powerful in overcoming this resistance and as a result are increasingly toxic; a fact that has been amply shown on this website. The idea of “killing the enemy”, bacteria, viruses, fungi and parasites, even spread to the treatment of cancer, the maverick cells that had to be eliminated. Does this first paradigm have its own limitations?
The Second Paradigm: Maintaining Host Defenses
Using the analogy of a fortress or castle, the question becomes very simple: can we assist the defenses of the body versus killing its enemies? The answer is equally simple———-yes! In order to explain this in a meaningful manner, I am going to liken the body to an old fashioned fortress. Fortresses were protected from hostile attack by thick walls that were surmounted by battlements. Sentries patrolled the battlements, watching for enemy attack. If such an attack was sighted, the first obligation of the guard was to notify the “keep”, the name given to the command post from which a commander controlled the defense. If the attack came from the west, off duty soldiers would be dispatched to the western battlements and the design of the defense would then require a stream of information by means of messengers between the command post and the areas of action within the castle. The castle would survive and remain intact only if the fighting soldiers were supported by additional services such as delivering ammunition, feeding them and replacing them with fresh soldiers when they were fatigued. Finally, the castle had to be designed originally and it probably went through a series of design changes over the years as it evolved. This is a fundamental rule in warfare, that the troops must be fed and rested, ammunition replenished. In human health, however, we have forgotten that rule. We have focused all of our efforts on the killing of the pathogenic enemies, with little thought to maintaining the health of our troops.
Consider the Brain and Body Castle
We know that the design of animal systems, including the human body, is guided by genes acting as a blueprint in which mistakes can occur. There is no doubt that we have evolved over millions of years to reach the kind of sophistication that we have today. The questions surrounding that evolution are by no means answered yet, but the complexity is so abstruse that it suggests intelligent design rather than chance.
The skin is the largest organ in the body, so think of it as being like the walls of a castle. It is dotted with sensory cells that may be likened to the battlements. Mucous membrane forms a protective layer over sensitive tissues like the nose. The lower part of the brain known as the limbic system can be imagined as like the “keep”. The upper part of the brain houses the commander.
Now, imagine bacteria alighting on the skin or the mucous membrane of the nose: the recognition of an “enemy” by the sensory cells results in a message being delivered to the limbic system of the brain. This part of the brain is a computer, receiving and sending messages to the body automatically. It is in constant communication with the upper brain. As the “ultimate commander” the upper brain is the thinking part, adding advice and consent to the ultimate action. Strengthening the limbic system, while weakening the action of the upper brain, most commonly achieved by poor nutrition, makes the ensuing action more primitive. The limbic system is the “caveman” within us all.
Organization of Host Defenses
Think of the white cells in the body as each being a soldier with a specialized function. They must be directed to the scene of the attack and a battle takes place between the white cells and the “enemy”. Like all analogies, it breaks down because body defenses are extremely complex, but I have tried here to establish a principle, that we possess sophisticated defenses that are organized by the brain.
For example, inflammation is used as a defensive process, controlled through the brain using the automatic (autonomic) nervous and endocrine systems to deliver the necessary messages. The whole defensive process takes place under the command of the brain, a most important factor that is much neglected in modern medicine. The brain/body coordinating mechanism in an emergency situation must be initiated as soon as possible and the resulting action requires a huge amount of energy, particularly by the brain. Because of this it is designed for short term use. The “illness” is the physical evidence of this coordinating mechanism going into action. An increase in circulating white cells means that the reserve “soldiers” are being deployed via the blood stream: the rise in body temperature is beneficial because it decreases the efficiency of the “enemy”. The associated feeling of illness makes us go to bed and rest, thus conserving energy required for healing. Remember that the misguided approach of using aspirin to reduce the temperature in a child with flu was responsible for the lethal disease known as Reye’s Syndrome.
How To Bolster Host Defenses
Under the heading of the second paradigm I said that we can indeed help the defensive procedure and that it was simple. By simple, I mean that the facts should be known by all. The first principle that we need to understand is a rough idea of how the body/brain works, as I have outlined. The second principle is an understanding of routine preventive maintenance through appropriate exercise, rest and nutrition. Like the troops defending the castle, our immune system cannot fight the enemy without sufficient resources. These resources include nutrition, rest and exercise, the forgotten elements in modern medicine.
Both of these principles require education, starting at the earliest possible age in childhood. We all need to understand that we have a health responsibility to ourselves and that the old proverb “prevention is better than cure” is one of the wisest statements that has ever been made. The science of prevention is embodied in the development of Alternative Complementary Medicine, a form of medical intervention based on the study of energy metabolism and how it is preventatively or therapeutically treated. It states that if the genetic blueprint is intact, leading to a complement of sophisticated defensive body/brain equipment, the stress of living in a dangerous world can only be met by an adequate formation of energy to run the equipment. This can only be supplied by nutrition.
A new science known as epigenetics is the study of how our genes can be manipulated by diet and lifestyle, so even minor genetic mistakes can be overcome by supplying the correct fuel. Much has been written about this in medical journals that have been casually ignored by mainstream medicine. That is why I claim that mainstream medicine has its “head in the sand”. Each time a new discovery is made, an attempt is made to find a way of manipulating errors in it through a drug rather than a possible lifestyle and epigenetic solution. Perhaps it is time to remember that health is about maintaining host defenses too and not just endlessly killing pathogens.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image created using Canva AI.
This article was published previously on Hormones Matter in October 2014.