Recently, I stumbled upon a 2006 editorial in the journal Cancer Epidemiology, Biomarkers and Prevention circulating on social media. It introduced research linking infant leukemia to maternal pharmaceutical and environmental exposures. Digging deeper into the research highlighted by the editorial and the studies published subsequently over the last several years, led me to a very disturbing conclusion: certain types of infant and pediatric leukemia may be largely preventable.
Infant Leukemia Rare but Deadly
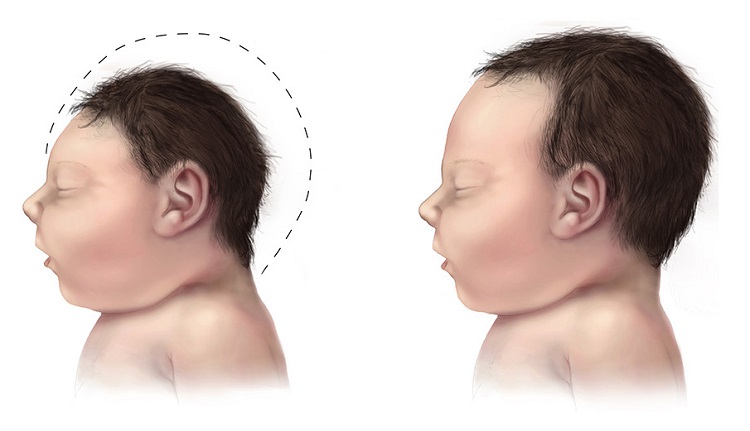
Leukemia in infants less than one year old is a rare, 41 cases per one million births annually in the US; but it is often deadly. Only 42% of infant leukemia patients survive beyond five years of age making it one of the more devastating forms of cancer. A large percentage (75%) of the babies with infant leukemia carry a specific mutation on the MLL gene at chromosome 11q23. The MLL gene is responsible for hematopoiesis or blood cell development. An error in blood cell development is at the root of this disease process, and unfortunately, it appears to be environmentally induced by specific, and increasingly common, in utero chemical exposures.
Infant Leukemia and the MLL Gene
Mom’s exposure to certain pharmaceuticals and environmental chemicals ‘rearrange’ the MLL gene and induce infant leukemia. This particular gene rearrangement, responsible for infant leukemia, and indeed, pediatric leukemia and cancer therapy-related leukemia (acute promyelocytic leukemia – APL), emerges in direct relation to chemical exposures, whether they be pharmaceutical or environmental. MLL- related leukemias are not heritable, not found in germlines, but a result of exposure in utero (infant leukemia) or during later child development (pediatric leukemia).
In recent years, a number of pesticides/herbicides, antibiotics (fluoroquinolones) and oral contraceptives and other synthetic hormones have been linked to the MLL gene rearrangement. When pregnant women are exposed to these toxicants, the result is a higher rate of infant leukemia, and I would suspect, miscarriage and infant mortality too, though this has not been investigated (see discussion below).
How Does Maternal Exposure Contribute to Infant Leukemia?
The primary mechanism of the MLL rearrangement associated with infant leukemia appears to be the inhibition of enzymes involved in DNA replication and repair. When a pregnant woman is exposed to these medicines or environmental chemicals, enzymes called topoisomerases, which are critical for proper cell division and DNA replication, are blocked. The errors that emerge from improper replication affect blood cell formation and induce the leukemia.
MLL and Topoisomerases
Topoisomerase inhibition induces the MLL rearrangements associated with most infant leukemia and a growing percentage of pediatric and even some adult onset leukemia. Topoisomerases manage the unwinding of nuclear DNA (nDNA) and mitochondrial DNA (mtDNA) when it becomes to tight to function appropriately (see short video below). The proper unwinding and re-attachment (scission and ligation) of DNA strands is critically important during cell proliferation. Proliferating cells cannot survive without functional topoisomerase enzymes. These enzymes are integral to embryonic, fetal and child development.
There are two types of topoisomerase enzymes active with nDNA (and many subtypes), type I (Topo I), which can repair only one strand of the double-stranded DNA and type II (Topo II), which can untangle both strands. Inhibition of either topoisomerase enzyme prevents DNA repair, but inhibition of topoisomerase type II, particularly type IIa, is deadly.
Additionally, there are three types of mtDNA topoisomerase enzymes that perform similar functions but within the mitochondria. Recall, mitochondria are the energy powerhouses of cells, responsible for supplying ATP, the fuel the powers cell function as well as a host of other important functions. Damage to mitochondria evokes a wide range of diseases. Most pharmaceuticals and environmental chemicals damage mitochondria via multiple mechanisms. Topoisomerase inhibition adds yet another hit to an already taxed system.
Topoisomerase Inhibitor Exposure Induces Infant Leukemia
A growing list of medications, vaccines, environmental chemicals and dietary components inhibit the activity nDNA and/or mtDNA topoisomerases, in some cases purposefully, such as with specific cancer treatments and antibiotics and others times coincidentally, as a side effect. Whether by design or by coincident, inhibiting topoisomerases creates long-standing health problems. When these enzymes are inhibited during critical windows of development, the outcomes can be devastating. To recap:
- A variety of chemicals inhibit topoisomerase activity, effectively blocking the enzyme’s ability to snip, unwind and correctly reattach the tightly coiled DNA during cell proliferation.
- Topoisomerase inhibition induces errors in the MLL gene that is responsible for blood cell development.
- MLL translocations are associated with 3/4 of all infant leukemia cases.
- Chemical exposures induce infant leukemia.
In other words, the connection between topoisomerase inhibition and the MLL gene rearrangement means that in up to 75% of the infant leukemia cases, the disease is not heritable, but rather, an environmentally induced in utero event. Sit with that finding for a minute, infant leukemia, a cancer with an exceptionally high mortality rate, is environmentally induced. Additional research suggests that up to 12% of pediatric leukemia’s, those with the MLL rearrangement, are also environmentally induced, post birth. Wow.
Medications, Pesticides, Vaccines and Dietary Items Linked to Infant Leukemia
- Oral contraceptives, anti-abortives and thyroid hormones. The Brazilian Collaborative Study Group on Infant Leukemia has published a series of studies addressing the various exposures associated with infant leukemia. Among them, a 2006 publication demonstrated that maternal use of synthetic hormones, (oral contraceptives in the early phase of pregnancy before the pregnancy was recognized, anti-abortive progestin treatments and/or thyroid hormones) increased the risk for infant leukemia 10X. The report did not specify specific brands or dosages of hormones. Other studies, reviewed here, link hormone use, or more specifically, the regulation of hormones and neural development, to the topoisomerase type IIB enzyme suggesting areas of interaction by synthetic hormone exposures.
- Fluoroquinolone antibiotics. It has long been known that the fluoroquinolone antibiotics are topoisomerase IIa inhibitors by design. We’ve reported on that here and here. Topoisomerase inhibition may account for many of the side effects associated with this class of antibiotics. During pregnancy, fluoroqinolones are associated with an increased incidence of fetal loss. Though not investigated, topoisomerase inhibition, nuclear and/or mitochondrial could be at play. Taken together, the use of fluoroquinolones in adults should be cautiously considered, but in pregnant women, infants and children, completely banned. Unfortunately, these are some of the most popularly prescribed antibiotics on the market.
- Acetaminophen. Metabolites of acetaminophen, the active ingredient in Tylenol (Paracetamol in Europe), is a noted topoisomerase II poison responsible for liver damage. Topoisomerase poisons act by different mechanisms compared to the inhibitors and are mutagenic and cytogenic. Preliminary evidence suggests the common use of acetaminophen to temper infant fevers developing post vaccine may be involved in the increased incidence autism, ADHD and other neurodevelopmental disorders while simultaneously reducing the antibody response to the vaccine.
- Pesticides. A 2013 publication The Brazilian Collaborative Study Group on Infant Leukemia addressing pesticides, reported that fully 60% of the children with acute lymphoid leukemia study’s catchment area and 36% of those with acute myeloid leukemia compared to 20% of the control group children were maternally exposed to pesticides, generally during the first trimester.
- Vaccines. We know that thimerosal is a topoisomerase inhibitor and that thimerosal remains in a number of flu and other vaccines despite the widespread belief that it was removed years ago. Notwithstanding the clear mechanistic capability, neither the role of maternal thimerosal or other vaccine exposures in infant leukemia nor the relationship between of infant vaccine exposures and pediatric MLL-based leukemias has been investigated. However, when we look at infant mortality in association with maternal vaccination, we see a striking increase of infant loss relative to vaccine uptake. A study published in 2013, tabulated the rate of infant death relative vaccination across the 2009/2010 flu seasons, as reported in the national registry for vaccine adverse events (the VAERS system). The data showed an “approximate fourfold (43%/11.3%) increase in the percentage of pregnant women vaccinated in 2009/2010 compared with 2008/2009,” that corresponded to “a 43.5-fold increase in fetal-loss reports – from 4 in 2008/2009 to 174 in 2009/2010“. The mean elapsed time between vaccination and fetal loss was 11.8 days with the mean vaccination time 13.8 weeks of gestation. It is conceivable, and mechanistically plausible, that vaccine induced topoisomerase inhibition contributed to the fetal loss.
- Maternal diet. A wide range of fruits, vegetables and other foods are topoisomerase inhibitors and in theory capable of inducing the MLL rearrangement associated with infant and childhood leukemia. A group of cancer researchers recently addressed this possibility, tabulating and calculating maternal intake of topoisomerase inhibiting foods across pregnancy. The results were quite interesting. Unlike the clear associations between the medications, environmental chemicals and the MLL – infant leukemia, eating foods that inhibit the topoisomerase enzymes didn’t always induce infant leukemia. Indeed, a diet rich in fresh fruits and vegetables, even those known to inhibit the topoisomerase enzymes, reduced the risk for infant leukemia, suggesting that with foods at least, the relationships are far more complicated.
Infant Leukemia is Rare: Do We Really Need to Worry?
While the worldwide rates of infant leukemia are low, at least apparently and relative to the scope and frequency of maternal exposures, one has to wonder if we are not missing other key components to this problem. Miscarriage, stillbirth and infant mortality rates have climbed in the US despite the presumed advances in medical care. MLL translocations, the cumulative effects of multiple pharmacological and environmental exposures are not investigated relative to these incidences. Vaccines and fluoroquinolones inhibit topoisomerase enzymes critical to cell proliferation, critical to embryonic and fetal development. Might the increased incidence of fetal demise associated with the administration of those medications be linked to topoisomerase inhibition? We’ll never know, but it is something to consider.
Is Infant Leukemia Preventable?
Perhaps. We need healthy and functional topoisomerase enzymes. Given the requirement for topoisomerase enzymes for cell development and DNA replication, preventing infant leukemia might be as simple as avoiding chemicals that induce topoisomerase inhibition during pregnancy. At least, 75% of the cases of infant leukemia are attributable to maternal exposures. As a mom, I find this both incredibly disturbing and hopeful at the same time. With current medical practices as they are there is strong push to prescribe medications and vaccines during pregnancy, without recognition of risk. It is this cavalier acceptance of drug safety that is responsible for so many health issues, and now, possibly, one of the most devastating cancers. I cannot imagine facing the possibility that a medication or vaccine encouraged by my physician was responsible for my baby’s disease and death. That is something no mom should ever have to face. I am hopeful though that the mamas reading this will be encouraged to stand up for their health and the health of their children, to do the research, understand the risks and the benefits of any medication or vaccine and make informed decisions. Perhaps a case or two of infant leukemia will be prevented as a result.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Cheryl Holt from Pixabay
This article was published originally on April 22, 2015.