For DES Daughters, Conception and Pregnancy Are Difficult
My first pregnancy, now 30 years back, was difficult. I am a DES daughter and after years of trying to conceive naturally, we tried in-vitro fertilization (IVF), which was pretty new at the time. The first IVF attempt led to a miscarriage. The second IVF attempt was successful and I gave birth to triplets. The pregnancy was difficult. I was on bed rest throughout the pregnancy and in hospital from week 26 through 30 when the babies were born prematurely. Although they were preemies and had to stay in the NICU for five weeks before coming home, they had few problems once they were home. They were all good nursers after they developed the sucking reflex at about thirty two weeks of age – two weeks after delivery. I nursed all three of them for the first six months and when they went onto solids they were great eaters.
A Miracle Baby but Something Was Wrong
Fast forward eight years, I became pregnant naturally. Something I NEVER in the world expected. This baby was such a miracle. To my surprise, the pregnancy was normal. I delivered what appeared to be a healthy baby boy via c-section. Early on, however, it became obvious that something was wrong.
My son, Austen had no interest in breast feeding and although the nurses said it was not an uncommon thing for a baby not to eat for the first few days. I remember being very concerned about his crying. Since, I had c-section, I stayed on at the hospital to get back on my feet. Austen wailed like only a hungry baby could. When he was taken from my room so I could get some rest, I could hear his cries in the little nursery down the hall, louder than all the others. The second day was like the first. Now I was worried. The staff seemed indifferent. He still wouldn’t eat and he was clearly unhappy.
That evening lying next to my bed in his little bassinet, his wailing forced me to get out of my bed to pick him up. The nurses were all busy and because it was a Friday there were a lot of visitors, noise, and rejoicing the birth of all the new babies.
Once I got Austen settled in my arms and I was comfortable, I tried once again to nurse him. Nothing. His crying turned to a sound that a little kitten would make. The light was low and I held him and tried to soothe my sweet little man. I don’t know if I fell asleep or we both became one again and my breaths were his and finally he was at peace. Suddenly my dream turned into a nightmare. I stroked his head and it was cold. I called his name and he didn’t move. I screamed at the top of my lungs for help and my baby didn’t flinch. I recall screaming forever until the room was full of people and lights and the hallway was silent. Austen was a strange blue color. They took him away and I knew he was dead and I still kept screaming.
My writer’s block is kicking in. This is where I always stop the scene running in my head. I can’t keep writing because I feel sick and clammy and the tears make it hard to see. I need to finish this story because maybe it could have a happy ending.
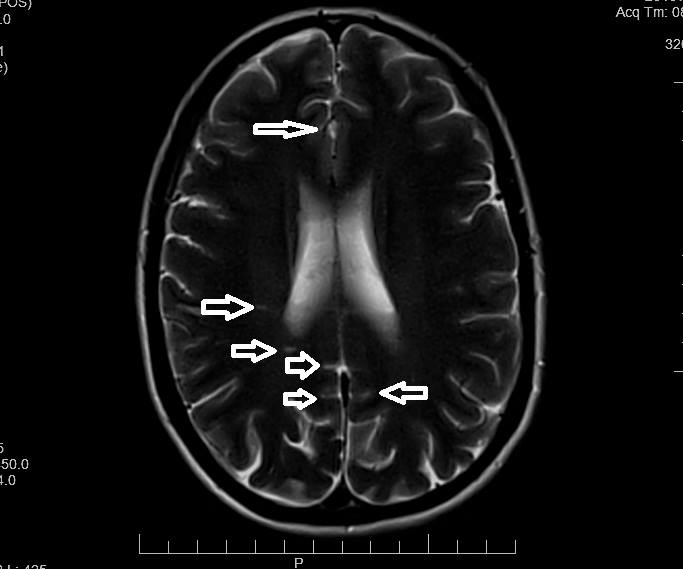
Austen was eventually revived. The nurses said he was without oxygen for twenty minutes. I think it was longer because no one came to my room to tell me anything and I was very hoarse from wailing. He was transported by ambulance to New England Medical Center, (also known at the time as The Floating Hospital for historical Boston reasons), where he was stabilized from the seizures and put under oxygen. Once again I had a baby hooked up to wires and tubes, but there was no excitement this time. He had suffered serious brain damage and on the third day of his stay in the NICU. I was asked to sit down with the doctors who had been following him.
The Diagnosis: Multiple Acyl CoA Dehydrogenase Deficiency (MADD)
Dr. A, the metabolic doctor who had been spending a lot of time with him, told me that he had a serious genetic defect. She called it Glutaric Acidemia type II or otherwise known as Multiple Acyl CoA Dehydrogenase Deficiency (MADD). She told me that it was a fatal disease and explained that he could not metabolize fats or proteins. She said that no other child born with this disease had lived for longer than six to eight months. She was patient with me when I cried. She said that she wanted to send a muscle fibroblast to a doctor in Iowa who would confirm the disease. She said that he could be brought home once he was taken off the tube feeding him through his nose and suck on his own. He should be given the best life possible in the next few months. It was “best not to resuscitate” should he stop breathing again, because of all the damage that he had already sustained. He was not to drink breast milk, too much fat and protein, so he needed a special formula.
The Power of a Mom Fighting for Her Child
Up to this point, I was in shock and depressed and felt very alone and defeated. But as I spent days with him watching as he came out of his long sleep and when he finally looked up at me and took formula from a bottle, something changed in my attitude. On the day we were told we could go home I became an angry, assertive woman, a person I had never been in my whole life. I demanded an apnea monitor to have at home in case he stopped breathing. I insisted that I would breastfeed him and I didn’t want the formula. After all if he was to be given the best life in six quick months, shouldn’t he be allowed to breastfeed?
He went home and I pumped and he learned how to nurse. I got in touch with the FOO (Fatty Oxidation Disorder) Family Support Group and the Organic Acidemia Support group and got a home computer. Austen grew. He gained weight and I became more determined not to let the diagnosis defeat us. We got the confirmation from the fibroblast that he had “2% of controls… as low as enzymes get.” It was a mitochondrial disease and there was no cure except to continue with the carnitine and B2 supplements that were supposed to sustain him.
I read Dr. Andrew Weil’s book, “Spontaneous Healing” and was particularly affected by the chapter that addressed malfunctions in DNA. He says that it can be reversed through diet especially by ingesting natural enzymes. I changed my diet radically after going to see a naturopathic doctor who put me on a meat-free, dairy-free diet which included mostly raw fruits and vegetables and whole grains, (both Austen and myself still follow this diet). I didn’t stop there, I sought out a Native American shaman, a Catholic priest who was a faith healer, a chiropractor… and a second opinion from another metabolic doctor.
A New Doctor and New Hope
From the first time I met Dr.K , I knew that we would be in good hands. He believed in treating Austen the individual, not the disease. His approach was much more hopeful and that is what I needed to keep going, especially since I was a single parent at this point. He marveled at his weight gain and cognitive abilities. He was delayed but he seemed to be progressing. The one concern was that his head circumference had come to a halt. Dr. K prescribed CoQ10 and in the next few months after starting it, his little head started growing again. Although he is still considered to be microcephalic.
When we started with solid foods each meal was traumatic, because he would throw it up from reflux. I had to clean up the mess and start all over again. I knew if he didn’t eat we would end up in the ER. He came to recognize that he had no choice in this food business, he had to keep it down!
I weaned him very gradually off of the barbiturates that he had to take for seizures and he has never had another one since. Ear1y on I recognized that Austen had a severe visual impairment and hooking up with Perkins School for the Blind got us involved with the infant toddler program, preschool, the ‘Lower School’ and last June he graduated to the ‘Secondary Program’. Social skills, PT, OT, sensory integration, mobility, music therapy, gym, arts, swimming and of course academics are only part of the total program. We had a skilled health care clinic on the grounds and were very lucky to live so close to the school and be part of this wonderful community.
Surviving Genetic Errors of Metabolism Through Diet
Today, at almost 22 years old, he is of normal height and weight, a handsome devil who is devoted to his older siblings, Nathan, Sasha and Taylor, and his loving stepfather, Joe. It has not been an easy road. We have had many bumps and starts. He stopped sleeping, (night and day) at about age three. Several trips to the ER after a vomiting bouts, severe sinusitis and airborne allergies, incontinence still to this day, but we persisted.
He has many food allergies which have been hard to decipher since he can’t really tell us ‘where it hurts’ and displays his discomfort through tantrums or negative behavior. Although once we got the nuts, legumes and lentils, etc., out of his diet, we have seen much less confusion and better spirits. The change in diet and recognizing that his behavior was on the autistic spectrum, (and getting the diagnosis of Asperger’s syndrome), has afforded me with much more knowledge of how to help my son deal with this world that he doesn’t really understand, and help others to understand his world. He is about to graduate from the Guild School for Human Behaviors where he has learned so much about how to express himself and keep his meltdowns to a minimum.
I feel strongly that the choices I have made for my son have been the right ones, but I could not have done it without the help of all the wonderful people I have met along the way, who now share a part of Austen’s world. Without them, I might not have made some of the connections that have made such a big difference in the quality of my son’s life. I cannot stress enough how important diet has been. The physicians in the NICU suggested that he would not live beyond 6 months and that we should not resuscitate should he stop breathing. I ignored them and with diet and persistence, he has lived and we have loved him for 22 years.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.