In our first post, Keto Dieting: Understanding the Basics, we discussed variations of keto dieting and looked at how keto diets affect clinical and non-clinical populations. Overwhelmingly, data suggest that there are health benefits for both populations. However, perhaps the most convincing argument against carbohydrate restriction and keto diets concerns athletic performance due to the athlete’s reliance on carbohydrate for fuel. In this post, we will investigate the role of keto dieting in athletic performance. As a matter of course, instead of searching for the “why or why not use keto as an athlete,” I prefer to take what is an obviously (to me) healthier diet and explore questions such as, “how many carbs can I eat on a keto diet … as an active person or athlete? or “can I optimize my performance while sustaining ketosis?”
The Use and Purpose of Dietary Fuels
Ketogenic diets are severely devoid of carbohydrate. Well, at least that is what we tend to think. From the diet’s inception, it has been restricted to 20-50g total carbohydrate per day. Only recently have a few individuals begun to question if that limit is necessary and under which conditions ketogenesis, and a greater carbohydrate, intake may occur simultaneously.
Why would we do such a thing?! If carbohydrates are bad, then they are just bad, right? And if they are bad, then shouldn’t we want to avoid them all. Period. While still less egregious than making the same association about fat, such as with the last nutritional paradigm, it is not a dichotomous situation. Carbs have a role. Fat has a role. I would argue that fat has a much more important role, but we cannot forget about carbohydrate altogether.
We have essential fats. We have essential amino acids. We have no essential carbohydrates. Still, they are widely considered the “base of human nutrition.” Since you can’t hear my tone in your head, read “base of human nutrition” with a low, sarcastic, and pompous sarcastic tone. In biological terms, “essential” means something that we need to eat because our bodies require it to survive and they cannot manufacture it on their own.
Put differently, without eating fat and protein, we die. Without eating carbohydrate, we don’t die. Are our lives rich and fulfilled? Maybe – it depends who you ask, how long they’ve lived following a carbohydrate-unrestricted eating pattern, their activity/athletic levels, and other factors. Some of you are thinking, “Hey! Fiber!” Fiber is not essential either. It’s fine; it’s just not essential. Sugar is not essential. Starch is not essential. Whole wheat is not essential. Not essential. Not essential. Not essential. Understand?
The Physiological Role of Carbs
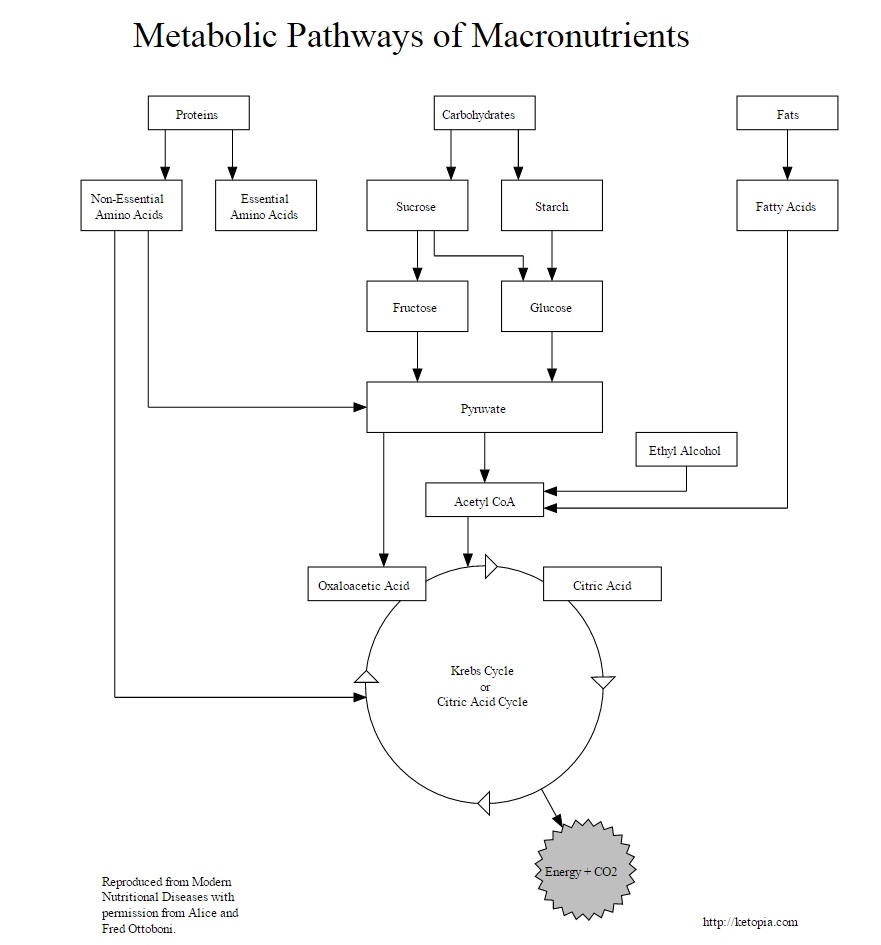
Just because they are not essential, does not mean they are useless. Carbohydrates are an energy source. They are used to make ATP, which our cells use to do all the cool things they do. Carbs are our “preferred” energy source because they don’t do anything else, and as a result of circumstance (eating high carb diets), they are observed as being metabolized at high rates – hence “preferred.”
Carbs make ATP now, or they are stored to make ATP for later. If muscle and liver cells are full of glycogen, carbs are converted to fat to be stored, but they are not as easily converted back. Luckily, our metabolisms are flexible, or at least, they are flexible as long as we don’t screw it up!).
Still, the creation of new glucose (gluconeogenesis) is possible, and this process can satisfy all of our carbohydrate needs. It is often said that our brain cells need more than can be supplied through this process. However, that is not entirely true. Humans can fast for hundreds of days and be just fine because any unmet carbohydrate needs are satisfied by ketones. That only leaves the blood cells which require carbs, and when we fast, all our blood does not dry up, so that theory doesn’t hold any water either.
An Evolutionary Aside
If we have essential fats and essential proteins, but we have no essential carbs, which do you think we evolved consuming? Which of the three were available in great enough quantity and frequency to support life such that we did not evolve the processes necessary to create them endogenously?
Bioenergetics, Briefly
Carbohydrates serve as an energy (calorie) source. Most of those living in the United States do not require any more energy than they are already getting. Over 70% of adults are overweight, and this number continues to increase. Calories in, calories out (CICO) is not a bioenergetic law, but it is still a rule that cannot be ignored. Eating too much still yields unpleasant consequences. However, we have to consider the calories out half of the equation.
We are only going to meaningfully increase calories expended (out) via exercise or other methods of physical activity. Certain types of exercise have specific dietary needs. One of the needs can be carbohydrate. There are levels to this.
At rest, we use a mix, about 50/50 to 65/35 of fat and carbohydrate, respectively, for our ATP needs (changes with training status, but even more with diet – up to 100% fat with carbohydrate restriction). As we start exercising, the rate of energy expenditure increases, but the mix stays the same. To a point.
As exercise intensity (speed, weight) increases, metabolic needs start to switch over to anaerobic glycolysis more exclusively. This means we burn more carbs. It’s not that we use less fat, fat burning increases until it “maxes out” then the extra energetic demand is made up from carbs. On a related note, the “fat burning zone” on cardio machines is not the most effective for losing body fat. It is simply an indicator of how fast as you can go before carbohydrate utilization goes up. Consider the recent popularity of HIIT style of exercise. This involves going way over the “fat-burning zone,” yet many feel it provides greater fat loss effects.
The point is that different exercise intensities utilize different fuel sources. At rest, we use about 50% fat 50% carbohydrate, and that changes to nearly 100% fat with keto-adaptation. During exercise, carbohydrates are still required when exercise intensity exceeds the “fat-burning zone.” In practical terms, if your exercise intensity makes you “feel the burn,” you’re using carbohydrates as fuel, and a lot of them. That is a great indicator that you are working hard. However, if the carbs are not available, you have a metabolic barrier to hard work – you can only perform the action if the fuel (carbs) are there to use.
Therefore when carbohydrates are in short supply, exercise performance suffers and higher intensity exercise performance, in particular, is impaired. However, with keto-adaptation, this does NOT appear to be the case. Nonetheless, most studies examining a ketogenic diet still find it detrimental to initial power output – the amount of force a muscle can create in an instant at the beginning of exercise. This adverse effect to power output is completely recovered once carbohydrate are added to a ketogenic diet. The trick is balancing.
A New Rule of Keto for Athletes
Referencing back to part 1 of this series, “a” ketogenic diet is not “the” ketogenic diet. Athletes, individuals with large calories (as carbohydrate) out, have a need for more carbohydrate, and they can maintain ketosis while meeting that need.
One of the first reports of this was indirect. Volek compared the metabolic characteristics of elite endurance athletes consuming a ketogenic diet or a typical high carbohydrate diet. The ketogenic athletes consumed over 80g per day of carbohydrate, equivalent to 10% of their total energy intake. Now consider variance. The exact data is 82 ± 62 grams per day. Thus, while some are keeping their diet strict – “the” keto diet – others are having success eating 140g per day (~2g/kg bodyweight) or more, as that’s only one standard deviation from the mean.
Keep in mind that these are ELITE endurance athletes. This is not for everyone. However, the study highlights a very important point. “The” diet has not been adapted for all populations, and it stresses that exercise, a healthy activity that we should all be doing(!), accommodates greater carbohydrate consumption.
As previously mentioned, my dissertation research included targeted carbohydrate intake as part of participants ketogenic diet. We tested escalating doses of carbohydrate in conjunction with exercise while participants were consuming a ketogenic diet as well. All participants maintained ketosis when consuming 20g pre-exercise, and some (about 10%) maintained ketosis consuming 60g. That is 10g over “the” diet’s limit in addition to the carbs consumed from the rest of their diet. They were eating about 1g/kg bodyweight or half as much as the athletes. As a percentage of calories, the carbohydrate-based controls ate about 50% carbs, 25% fat, 25% protein. The keto diets consumed between 5-15% carbs, 63-70% fat, and 22-25% protein. Ranges are provided to show the base keto diet as well as with the addition of 60g supplemental carbs. Most aspects of performance can be maintained with the base keto diet, but others, such as peak power output, needed at least the 20g added back in. Again, these data are in review.
Population sample is important. In the first example, we have elite athletes, and in the second example, recreationally trained college kids. Although I can personally guarantee that the participants in my study were trained hard, the workload does not compare to the best ultra-endurance athletes in the country. However, the information still helps us establish the pattern. Carbohydrates are activity dependent.
What Carbs Were Allowed?
Although a keto diet can be a carnivore diet, we generally still want to encourage sufficient vegetable consumption. Quick aside: you’re only allowed to be carnivore if you eat liver and other organ meats. In my work just described, all participants had a fiber goal, and in the keto groups, the fiber goal for the men was 18g and 15g for the women. While fiber is generally healthy, in research it is simply used as a marker to indicate diet quality, not so much for its own effects. Since fiber is fermented to fat anyway, I encourage the net carb calculation (total carbs minus fiber). Participants were instructed that the major contributors to their net carb counts should be nuts, seeds, avocado, coconut, olives, and low-carb vegetables, such as broccoli, celery, peppers, onions, salad greens, etc.
For those of you who already do that and want the “extra” carbs for performance, we used a pea starch called Carb10®, which is available as a supplement (disclaimer, I now sell one [as a result, not a cause, of the research] under Archetype Nutrition). I also recommend honey, rice, fruits, and even cookies as other options as long as you are responsible about it.
A Ketogenic Diet for the Healthy
In order to support different lifestyles, “the” diet needs to be adapted. We need to go beyond the rigid limits and let the diet be based on what it produces. A ketogenic diet can have all the characteristics and results of the ketogenic diet while permitting a more flexible and athletic lifestyle.
Encompassed within this, is metabolic flexibility in general. The standard American diet programs our metabolisms to use carbohydrate while “forgetting” how to use fat for ATP generation at high rates. Long term adherence to ketogenic diets can do the same in the other direction. A holistic approach to health involves diet AND exercise. The two are related.
Just as we would adapt a “normal” diet to support athletic activity by modifying carbohydrate consumption, we can modify a ketogenic diet. I would argue that we need to exercise as part of a ketogenic diet so that we can transition into a primarily anaerobic metabolism (that which is used to make ATP for high intensity exercise). We need it as part of any healthy lifestyle, but stick with me.
As previously stated, while keto-adapted we use fat for nearly all of our energy needs. The best way to maintain metabolic flexibility while keto-adapted is to periodically reintroduce carbs. The exercise creates the stimulus for those carbs to be used rather than stored. We train the metabolism to have duality, and we have no negative effects of carbs (such as fat storage, extended elevations in insulin/glucose, etc.).
For the athletes, or the physically active with performance goals, the inverse is true. The exercise isn’t necessary to manage the carbohydrates and metabolic flexibility, the carbs are necessary to support performance. They are the only fuel source that can be used to support high-intensity activity, and athletes need to train at high intensity.
What is the solution to this keto-carb dilemma? Eat enough, but not too much. It’s the same as everything else really. We’re just at a different point on the spectrum than we thought. The best time to eat more carbohydrate is near exercise, so they go in and get burned up without having time to be stored. They are just energy molecules after all. Use the energy, and it won’t be stored.
For the complete scoop on dosing carbs while keto, and for the other 4 new rules, read my e-book, The New Rules of Keto. It is totally free. It is free because these are the things I want you to know. I think it’s vital to the growth of the low-carb movement and our ability as a species to improve our quality and quantity of life! If athletes and other active individuals need not avoid ketogenic diets, is there anyone who should? Find out in part 3!
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.