If you have searched the Internet looking for health solutions, chances are you have come across warnings about the dangers of oxalates in some foods. You may even have seen a reference to something called a low oxalate diet. What does that mean exactly? What the heck are “oxalates”? Well, let’s explore that a bit.
What Are Oxalates?
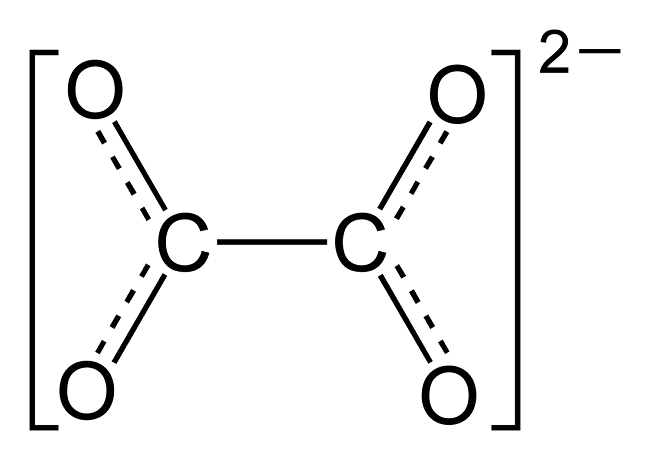
Oxalate is a relatively simple molecule in the grand scheme of things. Below is a diagram from Wikipedia.
Oxalate is present to some degree or another in virtually all plant foods, but almost totally absent in animal foods. Why would that be? To begin with, oxalate is not a problem for a plant. Plants use oxalate to help regulate minerals like calcium, which is a metabolic process essential to the health of the plant.
Calcium is a 2+ cation; oxalate is a 2- anion. That means calcium and oxalate are attracted to each other; one might even say they are “preferred dance partners”. That’s an important point because oxalate helps to bind with calcium and allows the plant to draw this needed mineral up through the roots. It can also be used to help to obtain other needed minerals, including magnesium (another 2+ cation). So that makes oxalate very useful to a plant.
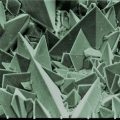
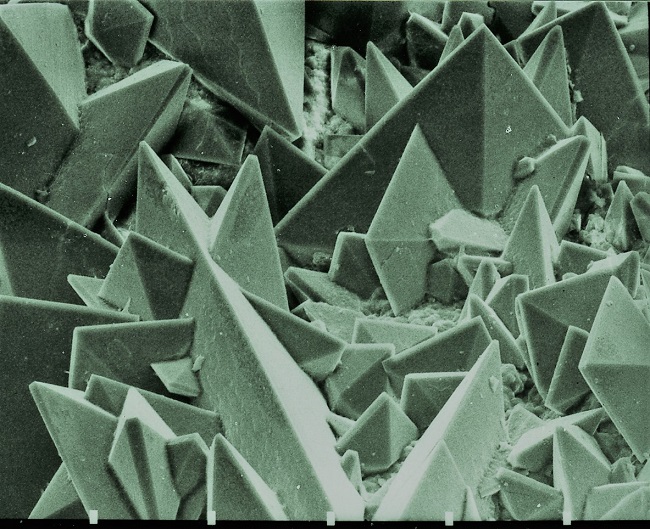
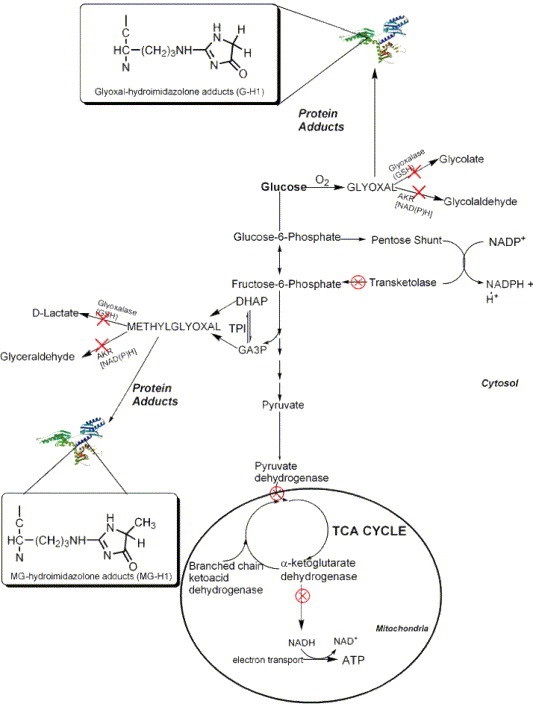
But this isn’t oxalate’s only purpose. In some plants, oxalate crystals participate in energy metabolism providing a source of carbon for respiration. In this case, oxalate may build up within the plant – but this is normal. Oxalate here may be protecting the plant from unfavorable environmental conditions, including drought and other stresses.
Plants have gone on to evolve other secondary functions for oxalate, including protection against both predation by insects and grazing by animals. One of these defenses can be the “Idioblast”. Idioblasts are specialized cells within the plant that may store plant chemical defenses, including oxalate crystals (as they do in the case of the Dieffenbachia plant). Oxalate may also be rich in the leaves of plants so that the mouths of insects may be damaged when trying to eat the plant.
Oxalates in Humans
The picture is vastly different for animals and humans alike. Oxalate has no useful purpose in the human body; instead, it can interfere both with our absorption and use of minerals, as well as with other important functions. The most commonly recognized issue that is directly related to oxalate is the dreaded kidney stone.
But that bias may be working against us; your general practitioner – and even your kidney specialist – may believe that the only issue with oxalate is the appearance of kidney stones. No stones? No problem!
For some, especially if their diet is not focused on the highest oxalate foods (see a list of the highest oxalate foods here), this may be true enough. For these folks, oxalate is a “mild” human toxin, as long as the intake is low enough, and the person is healthy. In this case, the body is able to clear it effectively, primarily through the kidneys. For other folks, however, consumption of even small amounts of higher oxalate foods presents significant problems.
Unfortunately, many of us are neither as healthy as we think, nor are our diets as low in oxalate as they were traditionally in the past.
Before the advent of modern food processing and shipping, many foods were seasonal and we simply couldn’t consume them in large amounts all year round. Good examples would be tender greens like spinach, which were eaten in season. Mind you, that might not have been enough to protect everyone from oxalate’s effects, and the fact that the historical record confirms the existence of kidney stones would be an indicator of that.
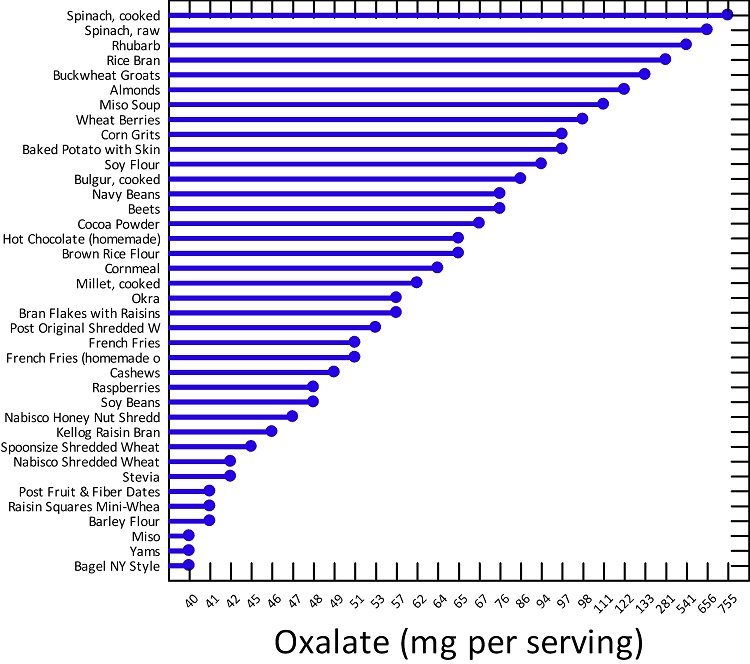
Another issue with the modern diet is that we often prefer foods raw; however, traditional cooking often saw certain plant foods boiled, which allowed oxalate to leach into the cooking water – which was then thrown away. With this modern preference for raw foods, we may unknowingly ingest extremely high oxalate in our diets. Research suggests that the daily oxalate consumption in western populations varies greatly, and can range as low as 44 mg/day and as high as 351 mg/day. Note that an average is smoothing out the highs and lows in intake, so your actual diet could range to extremely high levels. For instance, when extremely high oxalate foods like spinach, almonds, Swiss chard, beets, or rhubarb are consumed, your daily intake values may easily exceed 1000mg/day.
On one of the main support groups, Trying Low Oxalates, members report intake levels regularly in the area of 1000 mg a day. As a practitioner, I have personally seen oxalate intake as high as 3500 mg a day. If the individual is eating a Paleo low carb diet, and highly focused on leafy greens and nuts, reaching this level of intake is surprisingly easy. Keep in mind that hyperoxaluria – the condition of too much oxalate in the urine – is diagnosed at levels of oxalate in urine over 40-45 mg per day.
Where Do Oxalates Come From?
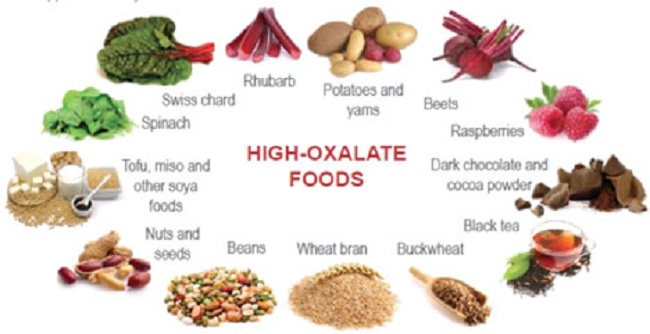
So where would the oxalate come from in your diet? Unlike other dietary exclusions, oxalate may be coming from a variety of sources, and each type of plant (and in some cases, even plant varieties) can have its own unique oxalate profile.
| Category | High Oxalate Foods |
| Beans/ Legumes | Anasazi, Black/ Turtle, Cannellini, Great Northern, Navy, Pinto, Soy (whole bean not tofu), White |
| Carob/ Cocoa | Dark chocolate, milk chocolate, chocolate substitutes using carob |
| Fruits | Blackberries, Mission/ dried Figs, Guava, Kiwi, Pomegranate, Rhubarb, Star Fruit/ Carambola, Cactus/ Nopal |
| Grains | Amaranth, Buckwheat, Quinoa, Teff, Wheat bran |
| Nuts | Almond, Cashew, Brazil, Hazelnut, Peanuts, Pine |
| Seeds | Caraway, Chia, Hemp, Poppy, Sesame |
| Spices/ Herbs | Allspice, Celery seed, Cinnamon, Clove, Cumin, Curry powders, Fennel seed, Nutmeg, Turmeric |
| Vegetables | Beets (root and greens), Bitter gourd, Burdock, Green beans (some varieties), Hearts of Palm, Jerusalem Artichoke, Okra, Plantain, Purslane, Potatoes (many), Sorrel, Sweet Potato, Swiss Chard, Spinach, Yam |
As you can see from the list above, it’s not as simple as just giving up nuts or beans. It can take a review of your overall diet to discover what the sources of oxalate are, and how much they are impacting you.
Among the more common high oxalate diets are those that use fruit and vegetable smoothies either for ‘cleansing’ or weight loss. People who consume these smoothies may ingest upwards of 1000 mg of oxalates per day, a high concentration for anyone, but one that becomes especially problematic if the individual has underlying health issues. Chronic health conditions often reduce the capacity to process oxalates. In these cases, high oxalate ingestion can become deadly.
Let us review a few of those ‘worst-case scenarios.
Considering High Oxalate Diets: Worst-Case Scenarios
Oxalate metabolism presents problems with high intake, especially when the individual’s health is compromised in any way. High oxalate intake alone can kill insufficient dose – although we don’t hear about it often. Recent case studies show us how easily dietary intake can take us into this dangerous range. We now have case studies of people – doing things that might be considered odd, but certainly within the realm of the ordinary – who then develop life-threatening issues.
The Green Smoothie Cleanse
Consider the case of a woman – well-intentioned – who began a green smoothie cleanse. Who hasn’t heard of such a thing in today’s world? Yet, after just 10 days, her kidneys failed. The green smoothie the woman was preparing contained over 1300 mg of oxalate per day, in spinach alone. Only her spinach intake is noted in the case study, although she may have had other oxalate sources, like nut milks or other vegetables. The material, in this case, indicates that the “normal” Western diet would have between 100 and 150 mg of oxalate per day. This is 10x the amount that the average person is getting daily.
Imagine drinking only green smoothies for days on end and on top of that having pre-existing health issues. Over 10 days, she would have consumed a minimum of 13,000 mg of oxalate. It becomes easy to see how her health might be comprised!
In this case, the woman had other risk factors: she was 65 years old; had undergone gastric bypass (a known risk factor for oxalate absorption); and, she had also taken several rounds of antibiotic therapy, which is also a risk factor.
Age alone compromises metabolism and excretion. Compromised metabolism due to age means that we find it harder to absorb needed nutrients from our food. Compromised excretion due to age means it’s harder to get oxalate out of the body once it is in.
If to the issue of age we add gastric bypass and antibiotic therapy, we have significantly altered gut bacteria and diminished our ability to absorb and metabolize foods. Indeed, bypass prevents normal absorption altogether, by bypassing a portion of the stomach and the intestines. That is its purpose – to reduce nutrients to the body to help the patient to lose weight.
What we see is that the combination of gastric bypass, antibiotics, and high-dose oxalate consumption can be deadly. It took only 10 days of what is a very common dietary protocol, to induce acute renal injury that could have progressed to full-fledged renal failure, had it not been caught.
Could a green-smoothie protocol induce such damage in other, healthier populations? Possibly. The variables that affect whether one has trouble dealing with oxalate are quite common.
It is well known that as we age, our ability to metabolize foods diminishes. One of the key things that we need to deal with the effects of oxalate is a good mineral level. Compromised digestion can easily compromise our level of many key nutrients, including minerals.
Antibiotics too, affect metabolism by disrupting the gut microbiota, and who among us has not been on multiple antibiotics over our lifetime? The likelihood that a person living in the Western world has had antibiotics is incredibly high. That means that our microbiome may or may not be ideal to handle dietary oxalate.
Then there is gastric bypass, which was performed on 179,000 people in 2013. This is a population whose metabolic function was already disturbed pre-surgery. Current statistics on the procedure are difficult to confirm, but given the US obesity rate was 38% as of 2015-2016, and appears to be rising, it is likely that the incidence of this procedure is rising.
Any one of the variables discussed (alone or in combination) would hamper an individual’s tolerance level for oxalate intake. If we then introduce an extremely high oxalate concoction like the green smoothie to the mix, it is entirely possible that oxalate issues will result, and that they will be serious.
Let us look at another case: a 51-year-old man on a low-carb diet, which also resulted in serious injury. Both “low carb” and “ketogenic” diets are very popular at the moment, although this particular vegan application was very strict and lacked protein. A low-carb protocol that included animal products would have meant less oxalate intake overall, as most animal products have no more than a trace of oxalate per serving.
This particular patient had done a protocol that included 6 meals of spinach, kale, berries, and nuts every day. With the current focus on eating more plant-based, it could seem healthy on the surface. Right? But here is the issue: not only was it excessively high in oxalate content, but the lack of animal protein and variety in the diet likely led to significant vitamin and mineral deficiencies, which in turn made the high oxalate content of his diet even more dangerous.
Finally, something as commonplace as star fruit consumption has been a cause of fatal injury in dialysis patients. Starfruit can contain as much as 300 mg of oxalate per 100 grams, putting a single fruit in the range of 270 mg. But that’s not as high as a single cup of raw spinach, which is over 300 mg for a single cup, eaten raw.
So what does this mean for us? While patients on dialysis have a clear risk factor, it may be surprising to note that there have been deaths in this population from consuming high oxalate foods. Note that as little as ½ a star fruit can be responsible for kidney injury for those who may have risk factors.
Not all risk factors are obvious either. How many people would adjust their diet because they had recently been on antibiotics? Once we are feeling well again, we would simply go back to our regular diet and all that is included.
Oxalate Consumption in Healthy Populations
This brings us to a discussion of those who are healthy. We might not be as “safe” as we think.
You may think that none of this concerns you because you have never had kidney stones and you do not have any of the pre-existing conditions noted in the case studies above. But as we saw from the green smoothie example, it is quite easy to reach excessively high oxalate consumption with common, everyday dietary practices.
Moreover, oxalate issues are not limited to kidney stones. Oxalate accumulation affects the entire body. In the second article in this series, we will explore oxalate consumption in ‘healthy’ populations and look at some lesser-known oxalate-related health issues.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Robin Higgins from Pixabay.
This article was published originally on September 16, 2019.