It is always amazing to me when seemingly disparate research articles come across my desk and within an instant there is a shift in understanding. That is what happened over the last two weeks, community members from different disease groups shared research articles. From the Gardasil community: CNS Demyelination and Quadrivalent HPV Vaccination . From our friends at Thyroid Change: Triiodothyronine Administration Ameliorates the Demyelination/Remyelination Ratio in a Non-Human Primate Model of Multiple Sclerosis by Correcting Tissue Hypothyroidism. And I connected some dots.
Thyroid and Neuromuscular Reactions to Gardasil and Lupron
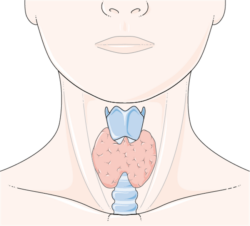
Among the more common side-effects reported by Gardasil injured and a group we are just beginning to study, Lupron injured women, include decreased thyroid function, sometimes associated with Hashimoto’s, thyrotoxicosis or even thyroid cancer. Simultaneously, but frequently viewed as separate or unrelated disease processes, both groups of women report a constellation of neurological and neuromuscular symptoms, many consistent with demyelinating disorders such as multiple sclerosis (MS). Indeed, case reports of central nervous system (CNS) demyelination or MS and Gardasil have been reported (cited above). There may be a connection between the demyelination process and the thyroid injury that develops as an adverse immune response to a drug or vaccine. More importantly, there may be a treatment opportunity.
Thyroid Hormones Affect Myelination
Almost a decade of research conducted solely in animals, rodents and monkeys, shows a connection between decreased thyroid function and demyelination disorders. Specifically, researchers found that administration of the thyroid hormone triiodothyronine (T3) not only improves the clinical course of the MS – like symptoms but effectively switches the disease process from a primarily demyelinating progression to remyelination. That is, the T3 induces cell level responses that regrow the protective myelin sheaths around CNS axons and corrects the medication-induced, tissue level, hypothyroidism. For the young women experiencing the host of neurological and neuromuscular symptoms post HPV vaccine, Gardasil or Cervarix, and/or post Lupron, this research may point to both an etiology and a treatment opportunity – disrupted thyroid metabolism mediated by an inflammatory reaction and T3 supplementation, respectively.
Dysregulated Thyroid in Critical and Chronic Illness
Vast amounts of research show a connection between thyroid function and critical and chronic illness. Hypothyroidism is common in what are otherwise considered ‘euthryoid’ or ‘normal’ thyroid individuals, but whose physiology is so severely stressed by disease or injury, thyroid function is affected. The presentation of diminished thyroid function during severe or chronic illness of unrelated etiology is often difficult to determine and its treatment is controversial. In these cases, thyroid stimulating hormone (TSH) is within the normal range in all but about 10% of patients and thyroxine (T4) may or may not be reduced. If and when further analysis is completed, T3, however, is often shown to be significantly diminished, the T4/T3 ratio is larger, reverse T3 (rT3), the T3 deactivating hormone is increased, while the enzymes responsible for converting T4 to T3 are reduced; clear evidence of disrupted thyroid metabolism that can be missed with traditional testing.
With the mixed laboratory presentation and evidence that supplementing with levothyroxine (synthetic T4) does little to improve patient outcomes, treating illness induced thyroid dysfunction is controversial, many physicians and medical organizations argue against treatment. Indeed, even in primary hypothyroidism, treatment with anything other than levothyroxine – T4 is controversial. Perhaps it shouldn’t be. The evidence reported in these animal studies, clearly indicates, T3 dysfunction and consequent supplementation controls the demyelination and remyelination process at the cell level and may improve clinical outcomes. In this research, T3 supplementation also improved T4 levels without a concomitant onset of hyperthyroidism, the reason often cited for not utilizing T3.
What This Means
If you or your child are suffering with the constellation of symptoms associated with an inflammatory nerve disease such as multiple sclerosis and/or if you have known hypothyroid symptoms in combination with undiagnosed neuromuscular symptoms, it’s time to connect the dots. The two may be related and may require T3 supplementation. Whether these symptoms were initiated with an adverse reaction to a medication such as Lupron, a vaccine such as Gardasil or Cervarix, or by some other process entirely, the research presented here clearly suggests a role for T3 in the array of symptoms associated hypothyroid disease and CNS demyelinating diseases.
Some of the symptoms associated with MS include:
- Vision problems (optic neuritis)
- Numbness or tingling of the face, arms, legs
- Chronic, unexplained pain
- Muscle spasms – painful muscle contractions
- Uncontrollable, often painful jerking of the arms or legs
- Extreme fatigue and weakness
- Dizziness
- Vertigo (spinning)
- Balance or gait (walking) problems
- Hearing problems or loss
- Seizures
- Uncontrollable shaking
- Breathing problems
- Slurred speech
- Trouble swallowing
- Dysfunctional bladder urinating frequently, strong urges to urinate, or inability to hold in urine
- Bowel problems – constipation, diarrhea, or loss of bowel control
- Memory problems
- Concentration problems
- Language/speaking
- Depression
- Rapidly switching moods
- Uncontrollable moods
- Inappropriate moods
These symptoms have been noted in post Gardasil or Cervarix reactions, and as we are learning, in post Lupron reactions as well. Even though these are two entirely different medications with entirely different mechanisms of action, the core reaction illness that ensues is inflammatory and often attacks the thyroid. When the thyroid is compromised, a range of other pathophysiological processes emerge, including demyelination. Certainly, additional research is warranted, but in the absence of time, and in the face of great suffering, T3 testing and supplementation may be indicated.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Markus Winkler on Unsplash.
This article was published previously on Hormones Matter in August 2013.