Even though women being prescribed Lupron (leuprolide) have, understandably, no clue about its adverse thyroid effects, it is no secret that Lupron adversely affects the thyroid gland. (The same could be said for adverse effects from Lupron on many other organs and bodily systems, but the focus here will be on the thyroid.) For decades, a wide variety of adverse thyroid effects during or following this drug have been reported to the FDA: according to RxISK.org’s compilation of Lupron FDA Adverse Event Reports (‘AERS’, for the years 2004 – 2014), Thyroid cancer, Hypothyroidism, Thyroid disorder, Thyroidectomy, Hyperthyroidism, Thyroid neoplasm, Thyroid function test abnormal, Autoimmune thyroiditis, Thyroid cyst, Blood thyroid stimulating hormone increased, Blood thyroid stimulating hormone abnormal, Blood thyroid stimulating hormone decreased, Anti-thyroid antibody positive, Thyroid cancer metastatic, Biopsy thyroid gland abnormal, Follicular thyroid cancer, Thyroiditis, and Thyroiditis subacute have all been reported (search “thyroid” in “Side effects reported” here; also Open Vigil, which contains FDA AERS for the years 2003 – 2013, can be searched.)
Different Warnings for Different Countries
For decades foreign labels for Lupron have identified “thyroid enlargement” as an adverse event ( i.e. 1998 Australian label for “Lucrin [Lupron]”, MIMS Annual 1998, Australian Edition, page 9-804; also 2010 Danish label – Danish Medicines Agency, Product Resume for “Procren [Lupron] Depot”). As early as 1986 the US product label for the initial formulation of Lupron (5 mg/mL vial, administered as 1 mg daily subcutaneous injections) identified “thyroid enlargement” as an adverse event (1986 Package Insert No. 3626, “Lupron/leuprolide acetate 5 mg/mL. Manufactured for TAP Pharmaceuticals by Abbott Laboratories, Rev[ised] Nov. 1986”; 1992 Physicians’ Desk Reference [PDR] , “Lupron/leuprolide acetate 5 mg/mL”, p. 2310). The US product label for the intramuscular injection of monthly Lupron Depot 3.75 mg (and other depot dosages) likewise identified warnings for thyroid enlargement (i.e., 1995 PDR, “Lupron Depot 3.75 mg.”, p. 2506; 1996 PDR – “Lupron Depot 3.75 mg”, p. 2558.) Between 2004 and 2012, there were 22 reported cases of thyroid cancer, and Lupron was considered “highly suspect” by a number of physician opinions, and according to RxISK.org’s FDA AERS database, there’s been 6 more cases (search “thyroid cancer” in “Side effects reported” here).
But, despite this history, all thyroid adverse events have been removed from the current labels of US Depot formulations of Lupron, and no thyroid warnings have been identified since the mid-2000’s – i.e., the current Lupron 3.75 mgs product label as well as the current labels for other depot dosages no longer contain any mention of thyroid adverse effects. The daily 1 mg formulation of leuprolide continues to identify warnings of thyroid enlargement and thyroid nodule, and foreign labels for Lupron continue to identify adverse thyroid effects, but the labels for US Lupron Depot formulations (which are prescribed the most for women with endo and fibroids) are devoid of any warning.
In the Courts
It is worthwhile here to revisit the atrocities committed during the only Lupron lawsuit to make it to trial (Karin Klein v. TAP/Abbott, Case 2:08-cv-00681-RLH-RJJ, 2011) – many prior lawsuits having been quietly settled with secrecy agreements. Karin Klein, at age 17, was prescribed Lupron Depot 3.75 mgs in 2005 when Lupron’s label no longer contained the prior-listed warnings about adverse thyroid events. Karin developed, among others, chronic autoimmune Hashimoto’s thyroiditis. Belatedly learning of Lupron Depot 3.75 mgs’ prior US label warnings of adverse thyroid effects, as well as the prior and current similar warnings in foreign labels, Klein sued for failure to warn.
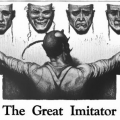
The judge at trial refused to allow the jury to learn of Lupron Depot’s pre-2005 US labels warning of adverse thyroid effects; the judge refused to allow the jury to learn of Lupron’s past and current foreign labels identifying adverse thyroid events; and the judge refused to allow the jury to learn of published medical literature identifying Lupron’s adverse thyroid effects (See Judge’s rulings, “Document 265, filed 07/25/11, page 13 of 40”, which can be found on p. 101 in this document). The judge would only allow the jury to learn of the 2005 US label. Moreover, Abbott’s mendacious defense medical “expert” stated under oath that “it was absolutely biologically impossible for Lupron to affect the thyroid gland. No textbook, no article has ever supported that contention. It’s simply biologically impossible.” (See “Page 20 of 131” here). A simple PubMed search shows this “expert statement” to be absolutely false – and this is without-a-doubt perjury (here, here, here and here). The first published report that “demonstrate[d] the association of thyroid disorder with leuprolide” occurred in 2000 – five years prior to Klein’s Lupron Depot prescription. Rhetorically speaking, exactly how does a paid “medical expert” get away with outright perjury concerning Lupron Depot’s – or any other drug’s – known risks?
This court’s curious restriction of limiting disclosure to only the 2005 Lupron Depot label (devoid of any thyroid warning) created the illusion for the jury that there were NO thyroid adverse effects from Lupron Depot for Klein to have been warned about — and so by a legal sleight of hand, Klein’s claim of “failure to warn” was made to disappear. The jury, unknowingly dis-informed and ‘educated’ in misinformation only, believed that it was ‘biologically impossible for Lupron to affect the thyroid gland’, and the jury found against Klein and found in favor of the drug company.
An appeal – bewilderingly – resulted in the Circuit Court making false statements and misstating facts. As argued on appeal by Klein’s attorneys:
“[Klein was] entirely shackled in the evidence she was allowed to present. It is particularly galling to have qualified (and expensive) expert witnesses on hand to testify, only for them to be shut down before the jury and precluded from offering competing expert opinions. The pattern shown by the record [of the Klein trial] is deeply disturbing. Virtually every discovery and evidentiary ruling, and other orders of significance, went for one party [TAP/Abbott and never for Klein]. … Such a one-sided proceeding was not the fair trial our system demands.” The multitude of rulings against Klein’s request for admission of evidence can be found delineated the afore-mentioned in “Document 265, filed 7-25-11”.
But the Circuit Court, in a 2-day deliberation, concluded: “… The district court did not abuse its discretion in excluding the challenged Lupron labels because they all contained information regarding the side effects of different formulations of Lupron, rendering them insufficiently relevant, unduly prejudicial, and likely to confuse the jury.” Here the Circuit Court misstates facts and conveys the opinion that “the pre-2005 US Lupron Depot 3.75 mg label for endometriosis” is a “different formulation” from “the 2005 US Lupron Depot 3.75 mg label for endometriosis”. This is utter hogwash from a high court – “Lupron Depot 3.75 mgs” is identical to “Lupron Depot 3.75 mgs” regardless of the year of the label. And it should not be terribly difficult for anyone (including the Court) to comprehend that the drug comprising the initial 1 mg. daily-injected subcutaneous Lupron was subsequently put into a “depot” (“long-acting”) ‘delivery form’, allowing one intramuscular injection to slowly deliver the same drug — Lupron – over the course of one (or three) month(s). The courts had access to the 2010 Danish label (Klein v. TAP/Abbott, Document 175, filed 06/12/11) in which it is stated “Leuprorelin [leuprolide] acetate is released at a constant rate over a period of 4 weeks (3.75 mg) or 12 weeks (11.25 mg) … which is equivalent with what is seen with a daily injection of 1 mg leuprorelin acetate.” (To date, I have not located that same statement in a US Lupron label.) This appellate court concludes that “Klein has not even remotely established that the district court exhibited such a high degree of favoritism or antagonism as to make fair judgment impossible.”
Denied her right to a fair trial a second time, Klein petitioned the US Supreme Court. One would (and should) assume the Supreme Court would inherently recognize the serious ramifications and public health impact of a case (any case) where perjury of the known dangers of a drug was committed by a defense expert (effectively hiding this information from the jury and ensuring a defense ‘win’), and where a Circuit Court completely misstated facts (upon which it had relied to deny Klein’s appeal). But, in fact, the denial of a plaintiff’s right to a fair trial, the denial of a jury’s right to truthful and accurate expert medical testimony, and the denial of society’s right to expect that court rulings will be based on authentic factual information were all issues the US Supreme Court deemed unworthy of review.
Broken Justice: Precedent for Medication Adverse Events Cases
These circumstances resulted in a devastating miscarriage of justice – not just for Karin Klein, but for all Lupron victims – and to society at large as well. What kind of precedence could this Klein verdict have upon future litigation – with this or any other drug? In fact, lawyers throughout the US, with potential plaintiffs seeking redress post-Lupron, were closely following the Klein case, and had Klein prevailed the floodgates of litigation were poised to spring open. But by securing a defense ‘win’ via, in my opinion, a multitude of highly questionable actions, those floodgates were slammed shut. (In May 2015 an RN disabled post-Lupron filed a lawsuit, and this case is presently making its way through the court system.) At least a few ethical and powerful legal experts should be examining the events in the Klein case – it could (and should) become renowned as a classic case of injustice personified. (Links to additional court documents and further details on the Klein case can be found at bottom of page, left column).
What does it mean when a young woman’s health and life are irreparably damaged and there is no recourse? How does a disabled victim fight against a system that has clearly indicated it is obfuscating and is the antithesis of justice? How does a society ensure that truth prevails, and harmful effects of drugs are exposed rather than shielded?
Recently, in attempts to achieve transparency in clinical trial data, many drug companies have put their clinical trial data online. The endometriosis clinical trial data for Lupron 3.75 mgs remains under a court seal – ensuring this data will never see the light of day.
There are many, many questions, and many, many victims, but as of yet – there are no substantive answers.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
If you have a Lupron story to share, send us a note: Write For Us.
This article was published originally on January 20, 2016.