Survey History
A few years ago, I embarked on a massive research project involving medication adverse reactions. I launched several online studies on the drugs that were popping up on our radar screen as having the most frequent and serious side effects; side effects that were largely ignored in the medical literature. At the time, this work was unfunded and, to a large degree, remains so today (feel free to contribute to our efforts). Despite the lack of funding, I thought it was important to investigate drug side effects from the patient’s perspective. Why was it that patients were reporting such a long list of devastating side effects while evidence in medical literature was largely absent? Were these patient experiences simply anomalies that we happened to be seeing, or was there something real going on? Without more quantitative data, these questions could not be answered.
To explore these questions, I designed several large studies, launched them online, and began collecting data, hoping that somehow the money would come in to fund the data analysis. It didn’t. And so these studies remained online, month after month, year after year, collecting data; data that needed to be analyzed and made public.
Earlier this year, I was fortunate to garner a grant for a new online project involving birth control and blood clots. The woman responsible for the grant understood the need to get the data from these legacy studies out to the public. The grant afforded me, not only the assistance of another researcher and a writer, but a much needed statistician. Per her wishes, the statistician could begin tackling the data analysis for these legacy studies, when not needed for the birth control project, e.g. during the periods of data collection. We are so very grateful that she recognized the importance of these projects.
A Note about the Data Sets
The surveys I designed were comprehensive, the data sets are massive and because they were conducted using survey software not designed for such large projects, the data sets are messy and require a tremendous amount of preparation to do even the most basic statistics. Notwithstanding the help of a part-time statistician, it will take us some months to ferret through these data sets. Nevertheless, we will get the data out. Again, if you’d like to help expedite this process, funding for a full-time statistician or even multiple statisticians would be most welcomed.
Beginning with Lupron
First in line, is one of my least favorite drugs used in women’s healthcare: Lupron. For those new to our blog, we’ve written a lot about Lupron over the years. Lupron or Leuprolide is a GnRH agonist prescribed for endometriosis, uterine fibroids, cysts, undiagnosed pelvic pain, precocious puberty, during infertility treatments, and to treat some cancers. I am not a big fan of this drug. If you have read the personal stories of the devastation caused by Lupron, or the research showing the mechanisms by which it induces damage, I doubt you would be either. Despite the decades of anecdotal evidence of serious side effects and the bevy of lawsuits filed and/or settled there is very little quantitative research delineating the scope and severity of these side effects. Given that Lupron chemically castrates its recipients, diminishing gonadal hormone production entirely, we might expect a little more research and certainly more caution in prescribing this drug. This doesn’t appear to be the case, as tens of thousands of women, men, and even children are prescribed this drug every year and have been for decades. Perhaps this is because Lupron is profitable, very profitable. In 2015, Lupron netted its manufacturers over $800 million in revenue.
What I find striking about Lupron, is not that are very few studies to support its safety and efficacy, or even that its manufacturers have been embroiled in lawsuits for decades all the while maintaining its safety and efficacy: that is common practice in the pharmaceutical industry. What is striking about Lupron is that it is a drug that effectively shuts down gonadal steroidogenesis, a key component of human health, and only a few in the medical industry think this is problematic. Here is a drug that could be used to induce chemical castration in pedophiles and rapists, if that were considered ethical or safe (and it’s not), but is used in tens of thousands of women, year in and year out, under the auspices of an effective treatment, and sometimes, even as a diagnostic for endometriosis. Worse yet, it is used on children in cases of precocious puberty, and to spur growth; two completely contraindicated uses.
How is that a drug that blocks hormones so completely, hormones that have receptors and therefore regulatory roles in every tissue and organ of the body (brain, nervous system, heart, GI system, fat cells, immune cells, muscle, pancreas, gallbladder, liver ) be considered safe? 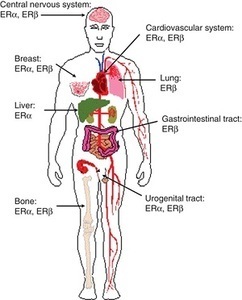 Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.
Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.
All snark aside, results from this project, and from our others studies, are critical to an emerging discussion about medication safety. Patient experiences tell us a great deal about drug safety and efficacy, if we ask. I think it’s high time that we begin asking.
Study Design
The Lupron Side Effects Survey was designed to assess potential side effects across all organ systems. Hormones have receptors everywhere: it stands to reason then, if we deplete those hormones rapidly and continuously, there will be effects wherever those hormones play regulatory or modulatory roles. Of course, since estradiol, the primary hormone affected by Lupron, is critical to mitochondrial morphology, and thus mitochondrial energetics, anywhere there are high demands for energy, the nervous system, the heart, GI, musculature, we might anticipate a high degree of effects in those systems as well, especially with longer term use and as the damage accrues.
What we didn’t know, and won’t until we fully analyze the data (what is presented here is only the beginning), is in which systems the side effects are most severe (do they follow the path of mitochondrial energetics or some other yet to be identified pattern ) and when (do they present early or late, relative to use?); which women were more likely to have side-effects (are there health characteristics that make side effects more likely or more serious?); is there a dose-response curve for side effects (do higher doses mean greater side effects – sometimes with hormones, this isn’t the case); or how the side effects cluster together (did they cluster by organ or tissue system or by some other variable, like energy demands?). Most importantly, we didn’t know whether Lupron was clinically effective at reducing the symptoms for which it was prescribed. There is some evidence to suggest that while pain symptoms associated with endometriosis may show a statistically significant reduction, particularly while the woman is taking the drug, the reduction was neither clinically meaningful nor long lasting. That is, symptoms may diminish by a few points on a pain scale while on the drug, but not abate completely, and then inevitably return upon cessation. In light of the potential side effects induced by this medication, one would expect nothing less than a large clinical reduction, even remediation of the disease process itself, as the only fair trade off. It is not clear whether Lupron can provide those benefits. None of these questions have been answered in the medical literature, despite the use of this drug for many decades.
Lupron Side Effect Survey Basics
The study was launched in 2013. The goal was to get 500 respondents, evaluate, redesign and relaunch follow-up studies. We reached the 500 respondents within a few months, but absent funding, were not able to perform the analyses. So I left the study up to collect data passively (no longer advertising it), until recently.
When we closed the study, we had over 1400 partially completed surveys. For robustness, we analyzed only those surveys that were over 90% complete. That netted data from over 1000 respondents (the number of respondents for each question varies and is listed below with each item). The survey was anonymous, voluntary, and included informed consent.
Survey respondents were asked to provide basic demographic information, answer questions about pre-existing conditions, reasons for Lupron prescription, Lupron dosage, and degree of efficacy pre, during, and post Lupron usage. To capture the range and severity of potential side effects, survey respondents were asked to indicate the presence/absence and severity of symptoms experienced relative to their Lupron usage with a 0-4 Likert-type scale (0=None, 1=Mild, 2=Moderate, 3=Severe and 4=Life threatening). And yes, we recognize that ‘life-threatening’ is not an appropriate indicator for some types of symptoms. For consistency, however, we used the same rating scale across symptoms. One hundred and eighty possible symptoms were assessed.
This post will review range and severity of Lupron side effects. Subsequent posts will address efficacy, side-effect clustering, patient characteristics predicting side effects, side-effect dose-response curves and other topics.
Demographics
Survey respondents (n=1064) were largely Caucasian – 86.6% (African American -4.7%, Hispanic -2.6%, Other – 2.3%, Asian – 2%, American Indian/Alaska Native 1.6%) and educated (30% – some college, 34% – BA/BS, 15% – MA/MS). The average age of the survey respondent was 35.36 (SD – 8.63), while the average age at which Lupron was prescribed was 29.9 (SD – 8.2). Among these respondents, Lupron was most commonly prescribed for endometriosis (88%), painful periods (33.5%), heavy bleeding (26%), ovarian cysts (18%), PCOS (4%), IVF (4%), anemia (3.9%), breast cancer (1%), ovarian cancer (.4%), precocious puberty (.2%), other (8%). Respondents could select multiple answers.
For the discussion that follows, see the interactive graphic below. We will be discussing symptom categories from left to right. The categories of side effects are grouped, to some extent, by system involved or by symptom characteristics. To view the side effects, click any of the boxes below. The side effects within that category will appear, along with the number of respondents who answered that question. Click again on a particular side effect and the severity of the side effect is displayed by percentage of women who experienced each severity level. Click in the white space within the graphs to move up a level (note, this is a little tricky in the categories with lots of symptoms). The size of the graphic does not display well on mobile phones and/or when using the internet browser Internet Explorer. For the best viewing, please use a computer screen.
Patient Reported Side Effects Associated With Lupron
General Side Effects and Allergic Reactions
Compared to the frequency and severity of other symptoms experienced in association with Lupron, side effects relative to the injection itself and those that would be characterized as allergic reactions, itching, swelling, etc., were uncommon in most of the respondents, except for injection site pain, which was experienced in varying degrees of severity by over 70% of the respondents.
Sex and Libido
As one might expect with medication that chemically castrates its users, reductions in libido and other symptoms whose net result diminishes sexual interest and ability were common. Some degree of a loss of interest in sex was experienced by all but 23% of the women, with 38% reporting a severe diminishment in sexual interest. Nearly 44% of respondents reported moderate to severe pain during sex which may explained to some degree by the almost equal percentage of women reporting moderate to severe vaginal dryness. Other symptoms reported included breast pain, swelling, and to a much lesser extent, discharge.
Muscle and Joint Pain
Up to 50% of the women reported moderate to severe muscle and/or joint pain. This is notable inasmuch as for the majority of the women prescribed Lupron, pelvic and abdominal pain associated with endometriosis is the driving factor for the use of this drug. It appears that we may be trading pain in one region of the body for another.
Gastrointestinal and Related Symptoms
Here again we see that a large percentage of women (from 15-50% depending upon the symptom) report moderate to severe gastrointestinal disturbances from nausea, vomiting and diarrhea through constipation and even bowel obstruction. Moderate to severe bladder pain was common (~31%) as was difficulty in urination (~19%) and bladder control (~18%). Since bladder pain and interstitial cystitis are co-morbid with endometriosis, it is difficult to determine if these symptoms were precipitated or exacerbated by the Lupron or simply associated with the endometriosis and thus, not remediated by the medication. We will attempt to disentangle those relationships with further data analysis and in subsequent studies.
Of note, gallbladder disease (~6.2% – all categories combined), gallstones (~3%), kidney disease (2%), kidney stones (4.5%) and renal failure affect a smaller but noticeable number of Lupron recipients. This consistent with adverse event reporting elsewhere. Similarly, non-alcoholic fatty liver was noted in ~6.6% of the survey respondents.
Bone, Skin, and Related Symptoms
Bone formation is particularly hard hit by the diminishment of estradiol. Bone related symptoms are some of the most commonly reported side effects ascribed to Lupron. Research suggests Lupron induces a 5-6% decline in bone mineral density over just 6-12 months of use. Read more on the mechanisms by which Lupron induces bone loss.
Almost 20% of the women who completed the survey reported some degree of osteoporosis, and 16% reported cracking or brittle bones, 42% reported toothaches (9% severe) and 26% had cracking teeth. Osteonecrosis was reported by 3% of the respondents. Skin and hair symptoms were common and affected a sizable percentage of the respondents as well. What we failed to ask about were fractures in the spine and pelvis or osteoporosis in the jaw; side effects that commonly appear in post Lupron discussion boards. We will do so in subsequent surveys.
Temperature Dysregulation
As expected by a drug that induces a rapid menopausal state, vasomotor symptoms with temperature dysregulation were prominent afflicting ~90% of the respondents. Severe hot flashes and night sweats were reported by over half of the study population.
Metabolic Symptoms
Estradiol affects insulin regulation and general metabolism, so it stands to reason that if concentrations are diminished significantly, metabolic disruption would ensue. Hypoglycemia was reported by about 15% of the women, while hyperglycemia was reported by about 6%. Similarly, increased hunger and thirst were prominent at least 50% of the population, along with rapid weight gain (mild 19.2%, severe 25.9%). In contrast, rapid weight loss was reported by 12% of the respondents. New onset diabetes, Type 1 and Type 2 was reported by ~1% and 2.8% respectively. As we perform more advanced analyses, we will try to more fully characterize the metabolic changes in different groups of women.
Cardiovascular and Respiratory Symptoms
We know that the estrogens and androgens affect heart function via multiple mechanisms, both at the receptor level and via more global changes to mitochondrial functioning. What we don’t know is what impact blocking those hormones so abruptly and completely and sometimes even chronically, has on heart function. Clinically, the results of this survey point to dysregulated blood pressure (BP – 12.5%) and heart rate or rhythm (24.7%) with a trend towards the elevated measures for blood pressure (24.4% – all, 13.3% moderate to life threatening) and heart rate (27.7% – all, 22% moderate to life-threatening. However, there was a noticeable percentage of women who experienced lower blood pressure (16.4%) and heart rate (6.1%). At least 10 women experienced a heart attack, 36 women developed mitral valve prolapse, 10 women developed blood clots in the leg and 8 women had pulmonary emboli. Difficulty breathing and sleep apnea were reported by 22.2% and 15.6% respectively. As we do further analyses we’ll be able to more fully characterize the pattern of cardiovascular symptoms.
Brain and Nervous System Symptoms
The next five sections of the graphic represent the scope and severity of symptoms associated with the nervous system. Though categorized distinctly for purposes of display, the distinctions are somewhat arbitrary as the symptoms within each category represent those related to the brain and nervous system. Arguably, many of the cardiovascular symptoms discussed previously may also represent nervous system symptoms, possibly suggesting some degree of autonomic system dysregulation.
Headache, Migraine, Dizziness, and Seizures. A large percentage of women experienced headache and migraine pain, frequently rated as severe or life-threatening (27.2% and 28.3% respectively). Dizziness was common (69.4%), as was vertigo (46.9%). Sleepiness (68%) and fatigue (87.3) were common, but interestingly, also insomnia (76.4). Seizures reported by 5.1% of respondents. Falling (17.1%) and difficulty walking (27.9%), perhaps indicating balance issues, were also reported. TIAs were reported by 11 women and full strokes by 3 women. (Nervous System Symptoms).
Myoclonus and Neuropathy. Shaking, jerking, numbness, spasms and tingling were experienced to some degree by 15%-35% of the survey respondents. A sizable percentage of women reported moderate to severe symptoms. Muscle weakness was reported by 11-34% of the respondents whereas limb and/or facial paralysis was experienced 3-4% of the women. (Neuromuscular, Sensory Perception and Motor Control).
Hearing and Vision Disturbances. Some degree of blurred vision was experienced by 46.5% of the women, with a little over 20% rating the symptom moderate to severe. Partial loss of vision was reported by almost 10% of the women, half of them indicating moderate to severe loss. Similarly, almost 20% reported some hearing impairment. Similarly, hypersensitivity to light or to sound was indicated by 35% and 37.5% respectively. (Sensory and Motor Symptoms).
Speech and Language Disturbances. Fully 20-50% of the respondents reported difficulty with basic communication, everything from difficulty speaking and finding words to difficulty understanding speech, reading and writing. (Sensory and Motor Symptoms).
Mood, Memory, Mental Health and Affective Behavior. The brain is a major target of and source for steroid hormones. Estrogen receptors are co-localized on neurons and affect neurotransmission, neurite outgrowth, synaptogenesis and myelin growth and estradiol is generally considered neuroprotective. The prefrontal cortex, hippocampus, and amygdala, responsible for regulating directed behavior, memory, and emotion, have high densities of estrogen receptors. Depleting estradiol would be expected to have a significant impact on these functions, and it did. It is here that we see some of the most troubling and least well appreciated (by the medical profession) side effects associated with Lupron. A significant percentage of women reported severe psychological disturbances ranging from depression and anxiety (>50%) to suicidality (15% severe to life-threatening). Visual or auditory hallucinations were experienced by ~12%, with >6% reporting moderate severe issues. Moderate to severe frontal cortex issues like dulled or inappropriate emotions, lack of motivation, impulsiveness were reported in 25% to over 50% of respondents. Moderately to severely altered mental states (delirium, disorientation, confusion) were reported by 6%-25% of the women. Moderate to severe diminishment in memory capacity was reported by at least a third of the women. This is in addition the difficulties with language reported above. (Mood, Memory and Mental Health).
General Impressions
Consistent with the case stories and patient comments on message boards related to Lupron side effects, the majority of women feel rotten while on this drug. This is to be expected given the global distribution of estrogen receptors. The brain and nervous system seem particularly hard hit. Again, this is understandable given the density of estrogen receptors in the brain and the modulatory role it, and other steroid hormones, play in neurotransmission. By depriving the estrogen receptors of their cognate ligand, estradiol, Lupron fundamentally alters brain chemistry, abruptly and thoroughly. Perhaps even more troubling, estradiol is required for mitochondrial functioning. By depleting estradiol, the mitochondria are impaired, and with that impairment comes a long line of compensatory mechanisms that will ultimately derail not only mitochondrial capacity but also the capacity of all of the cell functions that require healthy mitochondria. The fact that we see such severe side effects attributable to nervous system function would be expected with estradiol depletion.
We Need Your Help
This post was published originally on Hormones Matter on September 1, 2016. Since then, we have lost our funding to complete this and the other ongoing studies. We have enormous data sets like this one on medication adverse reactions waiting to be analyzed and published. Without funding, however, these data will never see the light of day. If these issues are important to you, please contribute. If you know of an organization or benefactor interested in understanding short and long-term medication and vaccine reactions, please refer them to us.
Yes, I’d like to support Hormones Matter.
Photo by Diana Polekhina on Unsplash.