I decided to be a surrogate after watching a birth story on TV. I felt like it would be a meaningful way to give back. I was adopted as an infant and I wanted to help another couple have a baby of their own. I did some research, found an agency, met a couple, and went through reproductive screening at a fertility clinic. They explained to me that they would give me hormone injections to artificially stop my body from releasing an egg. I was a gestational surrogate, meaning I only carried the embryo. The embryo was made from a donor egg. Once they confirmed that I had not ovulated they would begin giving me estrogen to produce a uterine lining. After two weeks, it was time for the big day, the transfer of the embryo to my uterus. The embryo transfer was successful and so for twelve weeks following I took a daily injection of progesterone.
I am ashamed to say that I did not do my research and I did not know exactly what I was taking, other than “hormones”. I recall the potential side effects being listed as headache, fatigue and hot flashes and that these side effects were temporary and would dissipate after I stopped taking the medication. I remember glancing over the package insert for the leuprolide acetate (Lupron) noticing nothing was too alarming.
Post Lupron Symptoms
I went on to deliver a healthy baby boy in May of 2013, his parents were thrilled and it was time to focus on me again, get my body back in shape and move on with my life. It was August when I had my first “attack”. I was feeling extremely dizzy and had tingling in my left hand so I went to my primary care provider. She could not tell exactly what was going on but felt that the dizziness was caused by allergies and the numbness in my left arm caused by carpel tunnel. She sent me home with an antihistamine and a brace for my left arm. Eventually my symptoms subsided and I felt perfectly normal.
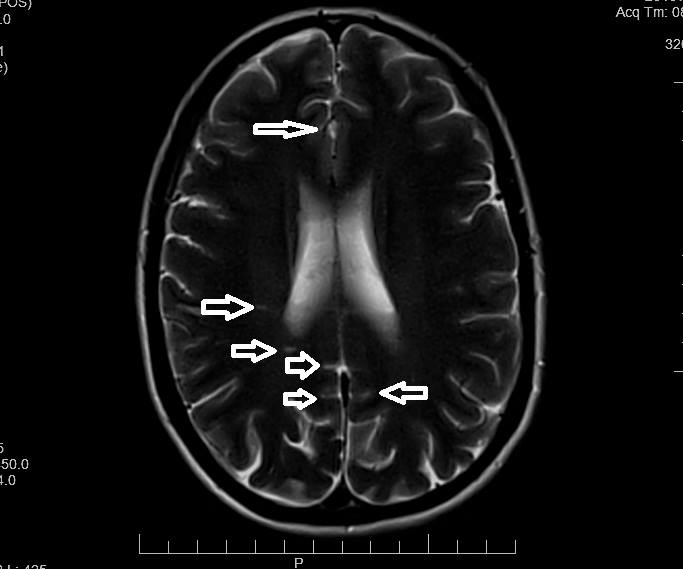
In January of 2014, I began feeling dizzy again, I tried an antihistamine and it just made me tired. The tingling and numbness came back in my left hand. I went to a different doctor who told me I had vertigo. The doctor tried a few tricks, such as hanging upside down and flipping up really quickly to try to “reset” my equilibrium (that didn’t work). The tingling in my arm was thought to be a pinched nerve in my neck because I lifted weights. Several days went by and I was still feeling terrible, the numbness was also occurring in my face. I was convinced I was having a stroke or that I had brain tumor. I went back to the doctor, insisting on an MRI. I was relieved when I was told that I did not have a tumor. The doctor said that I had signs of a demyelinating disease, such as multiple sclerosis. There are six lesions on my brain.
Multiple Sclerosis or Something Else?
Obtaining the actual diagnosis was a very long process which involved a lumbar puncture to check my cerebrospinal fluid for elevated levels of antibodies and a specific group of proteins called oligoclonal bands. The findings indicated I did have elevated levels of the antibodies but that the group of proteins were not present. Still the neurologist felt that it was enough for a diagnosis for multiple sclerosis and prescribed a disease modifying drug, a three times a week injection. Multiple sclerosis cannot be cured but there are drugs designed to try to prevent the immune system from attacking the myelin sheath (protective nerve coating). I sought the opinion of another neurologist who had a specialty in multiple sclerosis. She agreed with the diagnosis of Relapsing Remitting Multiple Sclerosis, which is characterized by clearly defined attacks of new or increasing neurologic symptoms. These attacks are followed by periods of partial or complete recovery. During remissions, all symptoms may disappear, or some symptoms may continue and become permanent. However, there is no apparent progression of the disease during the periods of remission.
Another Surrogacy and Another Round of Lupron
During this process, I knew that I was going to be gestational surrogate again. I had already committed to the couple to carry a second child for them. I stopped taking my disease modifying drug and began the gestational surrogacy protocol again of Lupron, estrogen and progesterone. Thankfully we were successful on the first round as we were with the first baby. Many surrogates are not successful on the first round and go through the protocol over and over again.
I was advised by my neurologist that many women have an exacerbation of MS after birth, as it is very stressful on the body. He advised that I begin taking steroids immediately following the birth to prevent a relapse. I had a very traumatic birth, resulting in surgery and I decided I did not want to take steroids. I would take my chances with the relapse – nothing happened, I felt perfectly normal again.
I am currently not treating myself with the medication prescribed for MS. I have not had any new or worsening symptoms in three years and each MRI shows no new lesions, although I live daily with existing symptoms. I have damage to my trigeminal nerve causing constant pain and numbness in the left side of my face, I also have occasional numbness and tingling in my left arm and leg.
When I was first diagnosed, I searched for nearly every cause I could think of. There is no one in my family history with MS. I didn’t have a vitamin D deficiency. I didn’t have the Epstein-Barr virus or any of the other things thought to be linked to multiple sclerosis. I started searching though my life for anything unusual, which is when I finally researched Lupron. There have been less than 5% of adverse effects reported; however, neuromuscular conditions are listed. I have since learned that there are no clinical studies on the safety of Lupron for IVF and it is being used as an “off label” medication. This allows for it to be used for medical purposes that were not originally specified in the FDA’s approval of the drug and it is not on the labeling. I have reached out to many women online and have heard similar stories of MS, or MS like symptoms or other autoimmune conditions and the use of Lupron.
I feel that I was lucky, I only took Lupron for a short amount of time, many women take it for much longer and at higher doses, possibly causing more damage. I want women, potential surrogates, reproductive endocrinologists and fertility clinics to be aware of this. I want more research to be done on the hazards of the drug. I want to prevent the off-label use of medications.
Share Your Story
If you have experience with Lupron and/or with surrogacy would like to share your story, send us a note.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on February 13, 2018.







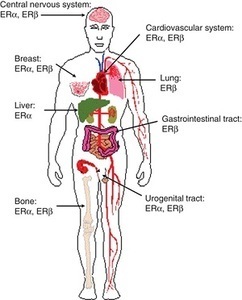 Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.
Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.




