After being prescribed Lupron for endometriosis and several IVF attempts during the years 1989 – 1992, I began to experience multiple symptoms and adverse health – virtually all of which were deemed by my physicians as “unrelated to Lupron”. But because there had been such an abrupt change in my health since taking Lupron, I strongly suspected Lupron was responsible, and so started scouring the medical, pharmaceutical, scientific, and government literature for any validating bits of information. Lupron (a.k.a. leuprolide, leuprorelin) is used on women, men, and children for A-Z indications.
Over the course of decades I visited nearly every university and medical library in Boston and had read countless studies and articles, accumulating a significant body of adverse information about Lupron’s effects and risks. Ultimately my health deteriorated further, and home-based internet searches replaced trips into libraries. All this information sat on shelves, doing no one any good, until finally in 2008 a friend created the basic website and the Lupron Victims Hub was born.
The Inception and Goals of Lupron Victims Hub
Lupron Victims Hub was founded in 2008 to serve as a central resource for information not otherwise readily found concerning the drug ‘Lupron’. Lupron (a.k.a. leuprolide or leuprorelin) belongs to a class of drugs known as “GnRH analogs/agonists” or the “relins” – i.e., Lupron = leuprorelin; Synarel = nafarelin; Trelstar = triptorelin; Zoladex = goserelin; buserelin; histrelin). Because of personal exposure to the relin, and the large market share that this drug has enjoyed, the website’s focus has been upon Lupron. To a lesser extent, the website also includes risks of other relins, as well as general risks to the relins/GnRH analogs as a whole.
The website exists as a resource for information on the risks and adverse effects of Lupron for consumers, medical professionals, attorneys, academia, and the media. All my research, information, support, and assistance has been provided pro bono. Contact from victims and families frequently centers on their search for doctors and lawyers to help them – but at present time there is no such ‘Post-Lupron doctor/lawyer referral list’. Hopefully the future will contain ‘Post-Lupron clinics’, with ample physicians and various specialties devoted to the diagnosis and care of Lupron victims – but currently, although there is a real nationwide need for such clinics, the thought is but a wishful pipe dream.
Twenty five years ago I felt like a lone voice, no one knew anything about Lupron, and no doctors or lawyers entertained a thought of this drug’s lingering adverse events. Now there are thousands of Lupron victims clamoring for help, lawsuits are in the courts and in the pipeline, and several physicians have gone on record about Lupron’s dangers, Lupron’s hidden data, and the serious permanent adverse effects upon women’s bodies. It would seem that a critical mass is being reached, more media coverage is occurring, and more and more doctors are in earnest trying to understand ‘what the hell happened’ to the health of their formerly vibrant patients.
It took me personally a dozen years of searching post-Lupron to find understanding, caring, and appropriate medical care – a totally unacceptable situation. When doctors and the FDA (see ‘Open Letter to FDA’ ) are uninformed of the drug’s data and risks, they are ill-equipped to understand or accurately assess Lupron’s effects. The atrocious “doctor visit stories” women recount post-Lupron (including my own) are hair-raising and nothing short of nightmare scenarios. Compassionate, diligent, and proper attention and care of these patients is urgently needed, yet negligently absent.
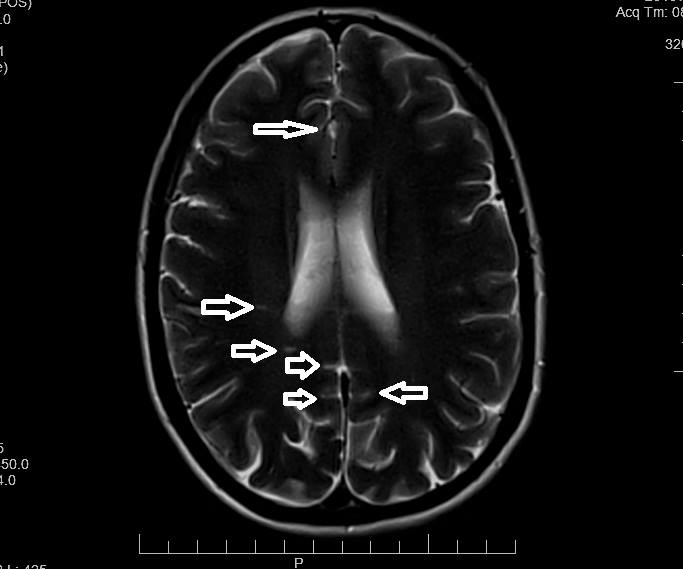
What We’ve Learned about Lupron
Information pooled on ‘Lupron Victims Hub’ should clearly identify that ‘Houston (and elsewhere) … “we have a problem”’. As for goals, I hope that my website will facilitate long-overdue acknowledgement of this public health crisis, and that those entrusted with our health and safety will initiate an investigation into Lupron’s long term adverse effects, remove the drug from the market, and establish appropriate medico-legal advocacy for these Lupron victims. And any order will do.
Participate in Research
Hormones Matter is conducting research on the side effects and adverse events associated with Lupron. If you have taken Lupron, please take this important survey. The Lupron Side Effects Survey.
To take one of our other Real Women. Real Data. surveys, click here.
To sign up for our newsletter and receive weekly updates on the latest research news, click here.
What Else Can I Do To Help?
Hormones Matter is completely unfunded at this juncture and we rely entirely on crowdsourcing and volunteers to conduct the research and produce quality health education materials for the public. If you’d like help us improve healthcare with better data, get involved. Become an advocate, spread the word about our site, our research and our mission. Suggest a study. Share a study. Join our team. Write for us. Partner with us. Help us grow. For more information contact us at: info@hormonesmatter.com.
To support Hormones Matter and our research projects – Crowdfund Us – Buy an Unsubscription.