It has been a year since I started taking high dose vitamin B1 (thiamine) for a variety of chronic symptoms including: Lyme disease, CFS/ME, endometriosis, histamine intolerance and other food intolerances, SIBO, chronic complicated migraine with aura, chronic insomnia, chronic severe light and exercise intolerance, to name a few. By traditional medicine, each of these conditions was considered unique and thus treated individually. I have learned that they are not separate conditions, but simply different manifestations of disturbed mitochondrial metabolism. In my case, all of this was related to deficiencies in thiamine and other vitamins and minerals. My recovery has been difficult and I have made many mistakes along the way, but hopefully, I learned from them. I am publishing my story here so that you may also learn from my experience. You can read my original story here.
Lesson 1: Magnesium Formulation Is Important
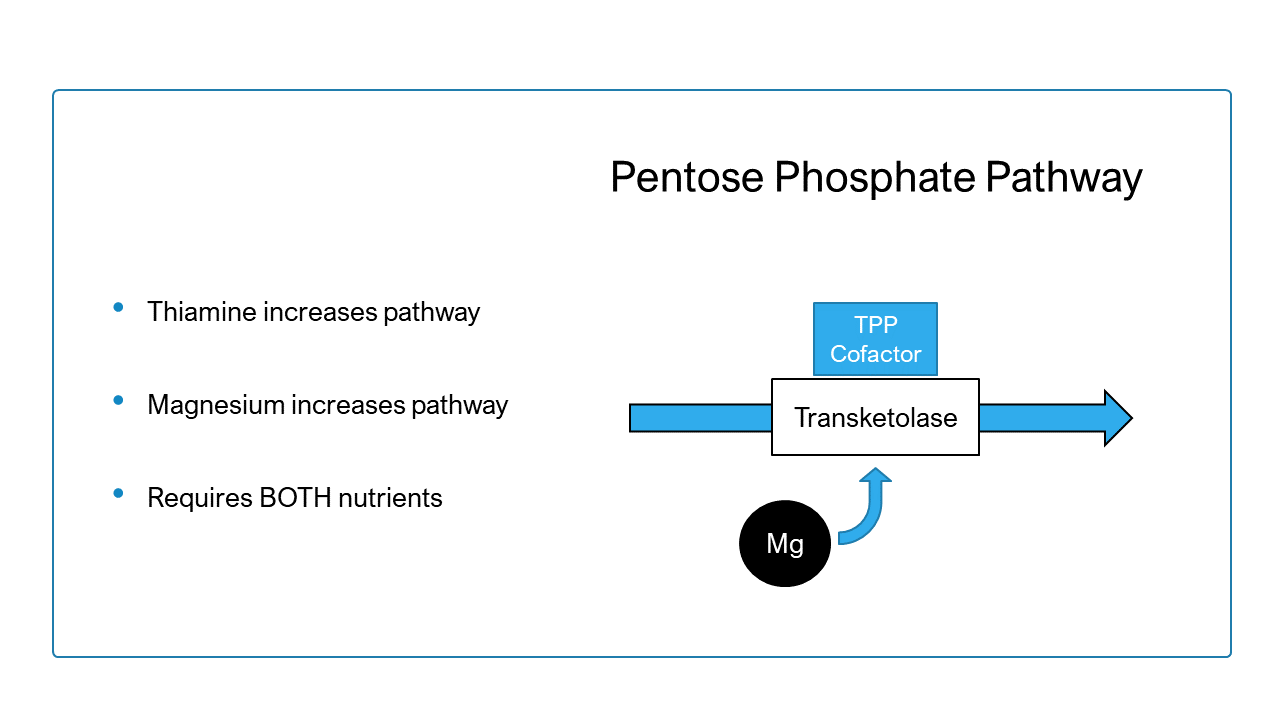
Magnesium is required to change thiamine from its free form to the active form called thiamine pyrophosphate (TPP). Without sufficient magnesium, supplemental or consumed thiamine remains inactive and basically useless. This means that magnesium deficiency can cause a functional thiamine deficiency. I understood this, but what I did not understand, was that there are many different formulations of magnesium supplement, each with pros and cons relative to the individual’s specific needs. I thought they were all interchangeable.
For me, and for individuals with heart related symptoms, magnesium taurate is preferred. One of my first mistakes I made was to ignore Dr. Lonsdale’s comments in which he talked about the importance of taking magnesium taurate. I understood it as meaning that magnesium was important and did not understand that it was a special form of magnesium with cardio protective effects due to the taurine content.
When I initially took magnesium taurate, I noticed an increase in my wellbeing, especially in the fatigue and headache that I would develop after walking around the house or being intellectually active, but I didn’t know that it was the taurine component that was responsible for that change. For a while, I stopped taking magnesium taurate and returned to using other forms of magnesium (magnesium citrate or malate). They did not help as much as the taurate. During this time, I also realized that I do not tolerate magnesium glycinate or bisglycinate. If I take that form, I have a terrible headache on the right side of my head. The glycine activates glutamate via NMDA receptors in the brain causing some excitatory activity. This may be why I could not tolerate it. Others do not have a problem with magnesium glycinate.
Over the last two weeks, I was that taking magnesium malate and taurine separately. I wanted to avoid spending a lot of money on magnesium taurate, so I tried to buy a cheap form of magnesium – magnesium malate – and combine it with taurine which is inexpensive when purchased in bulk. This did not provide the same benefits as magnesium taurate. I experienced chest pressure and pain and my resting pulse went back to being higher than 65-70 BPM. Once I began taking magnesium taurate again, my heart rate and chest pain/pressure disappeared.
So the lesson here, is that different formulations of magnesium work for different people. It is important to research which form may work better for you and your set of symptoms and not to assume they are interchangeable.
Lessons 2-3: TTFD Degrades with Heat and Light and Interruptions to Thiamine Repletion Cause Setbacks
One other important thing I realized was that thiamine is destroyed by UV light. This meant that in August, when I put my TTFD powder (a form of synthetic thiamine that crosses cell barriers more easily) in a transparent container on the kitchen table, and left it there all day long while sunlight shone directly on it through the big windows in my kitchen, it was being destroyed every day. I experienced a big crash during that month, especially since I was taking all the other vitamins and minerals that were serving as co-factors. I could not explain it and was thinking that even this therapy was losing its effect, that my recovery was over, and that I could no longer hope for a better quality of life.
However, in September, I received my new order of TTFD powder. The very day I received it, I took my regular dosage from this new batch. The difference was incredible in terms of my symptoms. It was night and day. The effects were truly remarkable and unmistakable. I’m very careful now with my TTFD powder and make sure it stays in an opaque container.
Lesson 4: Treating My Carnitine Deficiency. Once Again Formulation Matters.
Another thing that I had not been able to fix was my carnitine deficiency. This was discovered by the neurologist who suspected that I was dealing with a FAOD (fatty acid oxidation disorder) or a mitochondrial disease back in February. Free carnitine levels in blood are supposed to be between 17 and 49, while mine was 6. I tried taking various forms of carnitine (L-carnitine, acetyl-L-carnitine, l-carnitine tartrate, Optimized Carnitine, propionyl-L-carnitine) but they all had a laxative effect which was aggravating my symptoms. I asked my neurologist if there were injections with carnitine that could replace the pills, but was left to figure it out for myself. And I did.
Through much research, I found a form that worked for me. It is called Propionyl-L-Carnitine. This form of carnitine is a known agent that protects against ischemia – quote from the linked study:
Free CoA and propionyl-CoA cannot enter or leave mitochondria, but propionyl groups are transferred between separate CoA pools by prior conversion to propionyl-L-carnitine. This reaction requires carnitine and carnitine acetyl transferase, an enzyme abundant in heart tissue. Propionyl-L-carnitine traverses both mitochondrial and cell membranes. Within the cell, this mobility helps to maintain the mitochondrial acyl-CoA/CoA ratio. When this ratio is increased, as in carnitine deficiency states, deleterious consequences ensue, which include deficient metabolism of fatty acids and urea synthesis.
This form of carnitine has made a huge difference in my health, especially with one particular symptom – the wet cough that had accompanied my walking around the house since April 2021.
More Energy and Exercise Tolerance with the Correct Supplements
In October, I began taking magnesium taurate and I also added higher doses of potassium to my regimen, just to see if I tolerated them. I had taken rather lower doses of potassium on and off since starting high dose TTFD. One of the things higher potassium solved, was the aftertaste (or after smell) that I used to get with 300 mg TTFD. I know most people dislike it, since it’s a sulphur smell, although I never disliked it.
After about two weeks on magnesium taurate and higher potassium intake with every dose of TTFD, I began propionyl-L-Carnitine HCL and Optimized Carnitine again. I noticed that they no longer had a laxative effect and I doubled my dose of propionyl-L-carnitine HCL so that I was taking about 600 mg three times a day, combined with one capsule of Optimized Carnitine.
After about a week, I noticed that I had more energy. I no longer needed to eat every three or four hours, I no longer had dyspnea or wet cough during the day when I was walking around the house. All those symptoms speak of cardiomyopathy and were resolving with the supplements. I still need to avoid sleeping on my left side and instead sleep on an incline on my back to be able to sleep through the night, but it my sleep is so much better now. My headache, something that has tortured me since I attempted intermittent fasting in 2018, is now gone. This makes me think that the right-sided headache is one of the symptoms of my heart not being able to do its job properly.
One of the things that helps the most with mitochondrial biogenesis is exercise and it is highly recommended for people with mitochondrial disease. However, in many studies it is noted that if cardiomyopathy is present, then this therapeutic cannot really be used. This is important because many people recovered and improved their exercise intolerance, but still develop symptoms after too much physical effort and wonder what they could further do to improve their symptoms.
After finding the right supplements to correct my deficiencies, I’m able to walk around the house without it aggravating or triggering my symptoms. Prior to this, I was largely bedridden and would have flares every time I attempted to do anything. I have a device that measures how many steps I take and it shows that I walk at least 1000 steps per day when I do nothing and spend 95% of the day in bed.
Now I’m able to go out and walk around my apartment building, which is about 150 meters and do not suffer any consequence. I tried walking more than that and if I do, my main symptoms come back (insomnia, heart symptoms and headache). It is progress, but I still have a long way to go.
I am also capable of learning a little bit of German every day. While my memory is still very poor, at least what I learn “stays” in my brain and the knowledge/understanding of the language accumulates slowly day by day. Intellectual activity no longer triggers the terrible, hours-long headache it once did.
Improved Sleep: Correcting the “Histamine Bucket”, Insomnia, and Heart Symptoms
Since becoming ill, I have had insomnia, likely due to my heart struggling to maintain a constant rate and rhythm. One of the very first things I heard that could explain my constant awakenings especially around 2-3am in the morning is the theory of the “histamine bucket”. This theory argues that around 2-3 am, there is some shift in our body’s physiology and histamine is released. Thus, if you already have a lot of histamines in your body, due to mast cell activation or low DAO, your histamine bucket is full and it will make you wake up. While this is plausible, I do not believe it is sufficient to cause these early morning awakenings. It is not a cause in and of itself, but one of the many things that get dysregulated downstream after nutritional deficiencies are ignored for a period of time.
My chronic early morning insomnia began in 2015, when my thiamine levels dropped and the aggravated mitochondrial disease began to unfold. I remember waking up and I would feel my heart beating more strongly (though not pounding), sometimes I would hear a pulsatile “whoosh” sound in my ear. I would also feel weird sensations in my chest, though not pressure. During those months, I would experience on and off dyspnea while walking to my office. I didn’t think anything of it because I approach my health in the exact opposite manner people with real hypochondria do. I just thought it was a subjective “feeling”, thus not worthy of an inquiry into a possible objective cause for it.
The experience I had in the last few weeks with the supplements mentioned above makes me doubt that mast cell activation or histamine “bucket” overflow are the main causes of waking up constantly at 2 or 3 a.m. I believe it’s most likely connected with the impact histamines have on the heart – they are a known factor in developing heart failure and using antihistamines does help in preventing/postponing the onset of heart failure. This also explains why of all medications, antihistamines were the only ones that helped with a lot of my symptoms in 2016/2017.
When I started taking magnesium taurate, potassium in high enough doses and propionyl-L-carnitine, my heart symptoms improved and my sleep improved. Recently, I woke up at 3 a.m. and I immediately took a low dose of magnesium taurate and a little bit of potassium citrate. I fell asleep again in 15 minutes and in the morning I felt ok. In the past, when I would take something like L-theanine. It would force my body to go back to sleep immediately after 2 a.m., but I would feel much worse in the morning, more than if I just had insomnia.
Restoring Normal Heart Rate
One of the most important things has been reducing my resting pulse from 75-80 BPM to my normal, prior to 2016 resting pulse which used to be 60-65 BPM. I remember I used to complain about it and doctors or nurses just brushed me off. They would say that if it is under 90 BPM, then it is not a medical symptom of anything. I knew they were wrong, but how could I argue? Somehow these people in white coats think that heart failure or other cardiac diseases start out of the blue, when in fact these diseases represent years and years of ignored symptoms before the onset of the full-blown disease with typical manifestations is recognized.
Lessons Learned
Everything that helps my heart function better and recover faster improves all of my symptoms, no matter how much they may seem unrelated. This is what I observed about my own body and I encourage everyone to listen to their body and understand that all symptoms are related.
If one version of one supplement does not work, try another form and combine it with different forms and dosages of other supplements. By supplement, I understand all substances that are naturally found in food or produced by the body.
When I saw that simple forms of L-carnitine don’t have an observable effect, I simply started searching for better forms of carnitine and found propionyl-L-carnitine, which is the physiologically active form of carnitine. Why I looked for other forms of carnitine? Because I learned from experience that high dose vitamin B1, as thiamine HCL didn’t help, but that high dose Allithiamine (a formulation with TTFD) helped and still helps my body working again as it should.
I found taurine (again) by searching for supplements that improve heart failure symptoms. When I first heard about it while reading one of Dr. Lonsdale’s comments, I didn’t understand why it was important.
No one should ever quit trying to figure out their own matrix of symptoms. Begin with the vitamins and minerals, while at the same time addressing infections, limiting damaging diets, limiting exposure to toxic substances and so on. I firmly believe that all diseases with chronic fatigue involve some degree of mitochondrial dysfunction – inherited or acquired. The prototype documented, unquestionable illness that causes hundreds of symptoms, i.e. a multi-systemic illness, is inherited mitochondrial disease.
I know personally of two other people who were completely bedridden, suffering from constant light intolerance, having to live in my bed for two years with a sleeping mask all day and all night, unresponsive to any treatment or approach promoted by the online integrative medicine doctors and communities. I did not think I would ever be able to become house bound, not able to tolerate light, to think or cook for myself. The ability to no longer be bedridden and forced to live in total isolation in darkness and to be house bound is nothing short of a miracle. I owe that to thiamine.
Usually people who end up in that state for so long never recover because all known alternative treatments are exhausted and high dose thiamine for chronic illness is virtually unheard of. I will make sure to do everything in my power to change this, no matter the costs, because there’s just too much unnecessary suffering out there.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image created using Canva AI.
This article was published originally on December 9, 2021.













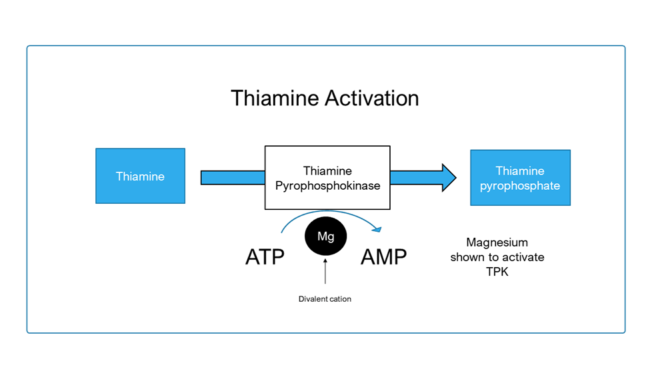 After absorption, dietary forms of thiamine gain entry into the cell through transport proteins. Once inside, free thiamine must be converted (or “activated”) into thiamine pyrophosphate (TPP), the biochemically active coenzyme form. This is achieved by an enzyme called thiamine pyrophosphokinase, which removes a phosphate from adenosine triphosphate (ATP) and attaches it to thiamine to make TPP.
After absorption, dietary forms of thiamine gain entry into the cell through transport proteins. Once inside, free thiamine must be converted (or “activated”) into thiamine pyrophosphate (TPP), the biochemically active coenzyme form. This is achieved by an enzyme called thiamine pyrophosphokinase, which removes a phosphate from adenosine triphosphate (ATP) and attaches it to thiamine to make TPP.