I have been reading some of the fascinating posts by Angela Stanton PhD concerning her research in migraine headaches. I regard the substance of her discussions as somewhat like dots on a chart that need to be connected. I learned a great deal about the chemistry involved in migraine. One of her comments that involves ion homeostasis in brain metabolism is fascinating. She noted that “serotonin is created by a normally functioning brain. Why it decreases or increases in the brains of migraineurs has always puzzled me. Should we not try to find out why?” That simple three letter word is the heart and soul of research and I believe that I may be able to add some information that might provide an answer.
Ehlers Danlos and Migraine
In one of Angela’s posts she discusses a subject which has been of interest to me for many years, the overlap of symptoms in disease. She noted that 60% of migraineurs have one type of Ehlers Danlos syndrome (EDS) and 43% of EDS have minor changes in DNA (SNPs) found in migraineurs. She concludes that they must be related. Over 70% of migraineurs have Raynaud’s disease and there is an overlap with EDS and Raynaud’s. Therefore, she concludes that these three diseases are variants. In fact, there is an association between EDS, Postural Othostatic Tachycardia Syndrome (POTS) and a group of conditions known as mast cell disorders. EDS-HT, (one of the manifestations of this disease), is considered to be a multisystemic disorder, involving cardiovascular, autonomic nervous system, gastrointestinal, hematologic, ocular, gynecologic, neurologic and psychiatric manifestations, including joint hypermobility. Many non-musculoskeletal complaints in EDS-HT appear to be related to dysautonomia, consisting of cardiovascular and sudomotor dysfunction. Many of the clinical features of patients with mitral valve prolapse can logically be attributed to abnormal autonomic function. Myxomatous degeneration of valve leaflets with varying degree of severity is reported in the common condition of mitral valve prolapse.
A woman, with what was described as a “new” type of EDS, died after rupture of a thoracic aortic aneurysm. Autopsy revealed myxomatous degeneration and elongation of the mitral and tricuspid valves. Patients with POTS, a relatively common autonomic disorder, may have EDS, mitral valve prolapse, or chronic fatigue syndrome and are sensitive to various forms of stress, as depicted in the clinical treatment of a dental patient affected by the syndrome. Dysautonomia has been described in the pathogenesis of migraine, featured by nausea, vomiting, diarrhea, polyuria, eyelid edema, conjunctival injection, lacrimation, nasal congestion and ptosis. In general, there is an imbalance between sympathetic and parasympathetic tone.
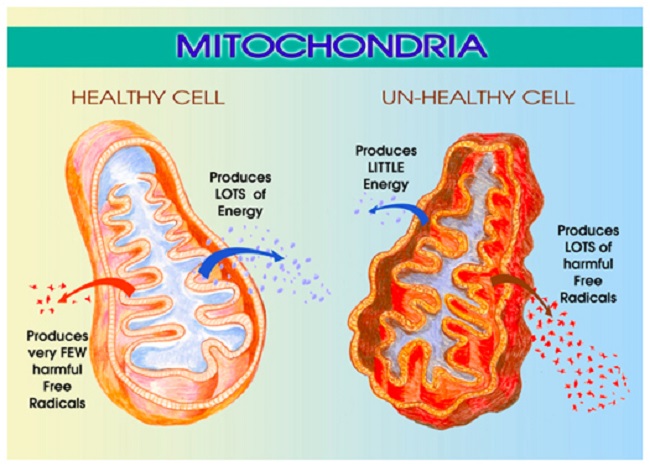
Energy Metabolism and Migraine
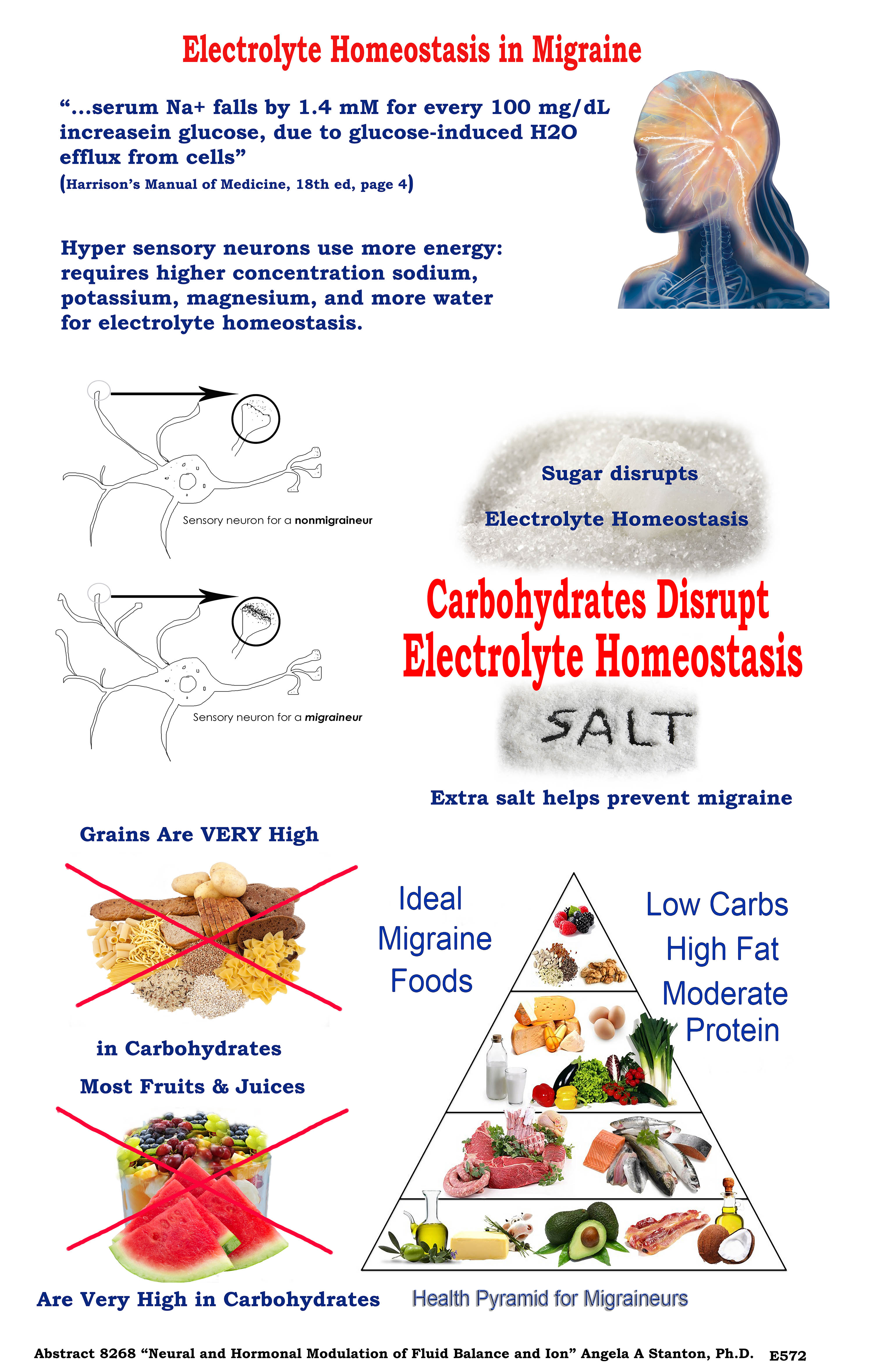
Technological studies have confirmed the presence of deficient energy production together with an increment of energy consumption in migraine patients. An energy demand over a certain threshold creates metabolic and biochemical preconditions for the onset of the migraine attack. Common migraine triggers are capable of generating oxidative stress and its association with thiamine homeostasis suggests that thiamine may act as a site-directed antioxidant. It strongly suggests that migraine is a reflection of an inefficient use of brain oxygen. An intermediate consumption of oxygen between deficiency and excess appears to be a necessity at all times. In fact,” moderation in all things” is an important proverb
Backing up energy deficiency, two cases of chronic migraine responded clinically to intravenous administration of thiamine. However, the authors are in error when they state in the abstract that “nausea, vomiting and anorexia of migraine may lead to mild to moderate thiamine deficiency”. An otherwise healthy 30-year-old male acquired gastrointestinal beriberi after one session of heavy drinking. Nausea, vomiting and anorexia relentlessly progressed. He had undergone 11 emergency room visits, 3 hospital admissions and laparoscopy within 2 months but the gastrointestinal symptoms continued to progress, unrecognized for what these symptoms represented. When he eventually developed external ophthalmoplegia (eye divergence), he received an intravenous injection of thiamine which reversed both the neurologic and gastrointestinal symptoms within hours.
In other words it is important to be aware that nausea, vomiting and anorexia are primary symptoms of beriberi due to pseudohypoxia in the brainstem where the vomiting center is located. Chronic migraine has a well documented association with insulin resistance and metabolic syndrome. The hypothalamus may play a role. One of Angela’s comments concerns ion homeostasis in migraines. Thiamine triphosphate (TTP) can be found in most tissues at very low levels. However, organs and muscles that generate electrical impulses are particularly rich in this compound. Furthermore, TTP increases chloride (ion) uptake in membrane vesicles prepared from rat brain, suggesting that it could play an important role in the regulation of chloride permeability. Although this research was published in 1991, the exact role of TTP is still unknown. It has been hypothesized that thiamine and magnesium deficiency are keys to disease.
Angela wondered why serotonin might be increased or decreased in migraineurs. I strongly suspect that it is due to brain thiamine deficiency as the ultimate underlying cause of the migraine. In a review of thiamine metabolism, it was pointed out that metabolites could be high or low according to the degree of the deficiency. Victims of beriberi were found to have either a low or a high potassium according to the stage of the disease. If they were found to have a low acid content in the stomach, treatment with thiamine resulted in a high acid content before it became normal. If the stomach acid was high it would become low before it became normal. Since low and/or high potassium levels may be found in the blood of critically ill patients, thiamine deficiency should be a serious consideration in the emergency room or ICU Thiamine deficiency may be the answer for the fluctuations of serotonin observed in migraine.
Redefining Disease Models
According to the present medical model, each disease is described as a constellation of symptoms, physical signs and laboratory studies, each with a separate etiology. The overlap discussed by Angela suggests that the various conditions nominated have a common cause and that they are indeed nothing more than variations. If energy metabolism is the culprit, it would make sense of the infinite variations according to the degree and distribution of cellular energy deficiency. EDS-HT, described above is reported as a multi-system disease, exhibiting cardiovascular, autonomic gastrointestinal, hematologic, ocular, gynecological and psychiatric symptoms as well as the joint mobility. It seems to be impossible to explain this multiplicity without invoking energy deficiency as the cause. People with prolapsed mitral valve and a patient with a “new” form of EDS, reportedly have myxomatous degeneration as part of their pathology and it is tempting to suggest that such an important loss of structure might well be because of energy deficit.
The controls of the autonomic nervous system are located in the lower part of the brain that is particularly sensitive to thiamine deficiency and beriberi is a prototype for thiamine deficiency in its early stages. Dysautonomia is frequently reported as part of many different diseases, offering energy deficiency as the etiology in common. Yes, it is true that thiamine is not the only substance that enables the production of ATP. Nevertheless, it seems to dominate the overall picture of energy metabolism. It has long been considered the essential focus in the cause of beriberi, even though all the B complex vitamins are found in the rice polishings. Milling and the consumption of white rice was the prime etiology of the disease when it was common in rice consuming cultures.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on June 22, 2020.