In this post I will try to indicate how you might detect cognitive changes in a loved one and how you might help defer the onset of severe neurological disease. Every person developing dementia goes through mild cognitive impairment first. A given symptom might be short-term memory loss, difficulty in finding a particular word or forgetting well-known procedures. We expect such changes in people in their nineties, but if they develop in the fifties, you can suspect that this is the beginning of dementia that is a disease, not normal aging.
What Do We Know About Dementia?
A study published in 2017 reviewed the observational studies examining associations between non-genetic factors and dementia. A total of 76 unique associations were examined, of which seven presented convincing evidence. They found an association with use of benzodiazepines (common drugs for mental disease), depression at any age, late-life depression and infrequency of social contacts for all types of dementia. Late-life depression and type 2 diabetes were associated with onset of Alzheimer’s disease (AD). Emotional stress causes brain function that consumes energy.
A review assessed the effect of the drug metformin (used in the treatment of type 2 diabetes) on the risk, progression and severity of AD and other forms of dementia, as well as any measures of cognitive performance or impairment. A case of encephalopathy (brain disease) occurred in a patient receiving metformin who was in end-stage diabetic renal failure. The drug was withheld and signs and symptoms quickly resolved. The authors hypothesized that metformin induced thiamine deficiency (TD), based only on their use of brain imaging that has a characteristic pattern caused by TD. Although metformin has become a drug of choice for the treatment of type 2 diabetes, some patients may not receive it “owing to the risk of lactic acidosis (increased concentration of lactic acid in blood or urine)”, a significant finding in critically ill patients who often respond to thiamine administration . Diabetic patients taking metformin may be predisposed to thiamine deficiency that is common in diabetes anyway . There is epidemiological evidence linking type 2 diabetes and its related conditions (obesity, insulin resistance, metabolic syndrome) to AD and it has recently been proposed that AD can be considered as “type 3 diabetes” because of disturbed glucose metabolism in that disease .
Mental Versus Physical Disease
It is probably absurd to separate the body from the brain. As has been said on this website many times, the body is composed of between 70 and 100 trillion cells, all of which have individual responsibility. I have used the analogy of a symphony orchestra where the brain is the conductor and the body organs are like banks of instruments that have to work together. The cells in each organ can be compared to the instrumentalists. They all know what to do but must work together “to play the symphony of health” under “the baton” of the “brain conductor”. Hence, for example, the immune system is an extremely complex union of mental and physical, requiring the brain, the nervous system and a variety of cells that carry out function. Assuming that the genetically determined genome”blueprint” is perfect (without mistakes in the DNA) all the cellular machinery requires is energy and that comes from an enormously complex list of nutrients.
Resulting from a great deal of personal experience and the genius of Hans Selye, I have concluded, like him, that energy metabolism is the focal point of health and disease. Selye developed the idea of what he called the “diseases of adaptation”. He coined the phrase the “General Adaptation Syndrome (GAS) in which he described the processes by which an animal adapts to physical and mental impositions of stressors. A stressor is any form of threat encountered by us on a day-to-day basis. It may be mental (a divorce) or physical (infection, trauma). He concluded that energy was required to drive the GAS (the ability of the brain/body orchestra to face the stress and adapt to it). One of Selye’s students was able to support this idea by producing the GAS in an experimentally induced thiamine deficient animal. The remarkable thing about this work was that in Selye’s time, little was known about energy metabolism. Today, the biochemistry is well outlined, if not complete, and thiamine stands out as a vitally important component. In continuing the analogy of the orchestra, I have nominated it as “the leader” (the chief violinist in an orchestra).
The Demands of an Active Brain
By far and away the best example of an energy defect in human disease is that of thiamine deficiency beriberi. Because energy deficiency is the underlying cause, it can imitate virtually any collection of symptoms that are regarded as those of a specific disease in the present medical model. Also, because it has many “psychological” symptoms, a long morbidity (continuation of symptoms) and a low mortality, it is dismissed as trivial. Since the brain and heart are the most energy consuming organs, it would be an obvious conclusion that a well endowed functional brain (genius) might be more at nutritional risk than someone less well endowed. I turned to the medical histories of three historical characters, all of whom were acknowledged geniuses. Their health problems have been debated without any conclusions. It was their similarity that appeared to me to be so striking.
Charles Darwin
His medical history is discussed online. Apparently he suffered repeatedly throughout life, suggesting “genetic risk”. His symptoms included chest pain, heart palpitations, stomach upsets, headaches, malaise, vertigo, dizziness, muscle spasms, tremors, vomiting, cramps, bloating and fatigue, all described in beriberi. He was treated by a Dr. James Gully, whose therapy included “a strict diet” that was reported to give Darwin “improvement in his symptoms”. In September 1849 his symptoms increased, apparently “during the excitement of a British Association for the Advancement of Science”. Excitement is a brain perception whose function elevates the brain from a resting state and requires increased energy to adapt. Between the ages of 56 and 57 symptoms were reportedly continuous and the text described “copious and very pallid urine”. Cellular energy is dependent on an efficient consumption of oxygen (oxidation) and the yellow pigment that gives urine its characteristic color is known as urochrome, an oxidation product of hemoglobin. It suggests that the pallid urine may well have been an indicator of decreased oxidative function. Perhaps we can hypothesize that the exacerbation of symptoms related to virtually any form of stress may well have been from a combination of dietary deficiency and genetic risk.
Mozart
The medical history of this genius is less clear online than that of Darwin. He suffered poor health throughout life, again suggesting genetic risk. Between 1789 and 1790, the symptoms described were weakness, headaches, fainting and hyperactivity and he reportedly had many falls. A left temporal fracture was described in his skull, examined after his death, suggesting a fall injury. Also, it was reported that “drinking was a well-known weakness of Mozart”. The association of alcohol with thiamine deficiency is well documented. It produces functional changes in the automatic brain controls of the autonomic nervous system that might not necessarily result in loss of intellectual function, at least in the early stages.
Beethoven
His medical history is also less clear but apart from his well known deafness, the text reported repeated diarrhea, abdominal pain, migraine, rheumatism, nosebleeds and he died in delirium at the age of 56.
Of course, I am well aware of the multiple theories to explain the medical problems of these three geniuses. My point is that the workload exercises the brain and its function requires energy. It seems reasonable to suggest that the brain of a genius requires more energy than one less well endowed. Furthermore the passion that goes into the work often makes diet a secondary issue that is frequently neglected by such individuals. In the case of Mozart, the depletion of thiamine by alcohol would also have a deleterious effect on energy metabolism.
Neurodegenerative Disease and Thiamine
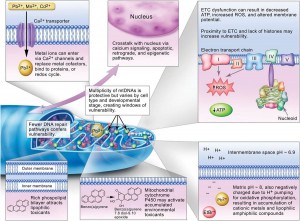
We know that thiamine metabolism is involved in the pathology of Alzheimer’s and Parkinson’s diseases. This has been shown in many papers published in the medical literature. An Italian doctor by the name of Costantini has published a number of manuscripts using high-dose thiamine in no less than seven different disease conditions, most of which are described as neurodegenerative diseases. Obviously, this is extremely offensive to the present medical model that believes each disease has a separate cause demanding specific treatment for each. If we look at the biochemistry of the human body, think of its complexity, its extraordinary dependence on a combination of genetic integrity, nutrition and lifestyle, it becomes easier to understand how a single molecule (thiamine) can be so vital. It stands at the gateway of the biochemical machinery that synthesizes energy in the form of ATP.
What is Energy?
Let us take a very simple analogy, that of rolling a stone up a hill. The point is that energy is consumed by overcoming the force of gravity trying to keep the stone at the bottom of the hill. We are imbuing it with what Newton called “potential energy”. When it gets to the top of the hill a simple push can cause it to roll down the hill and this would be referred to as “kinetic” energy. Although the principles in the human body are exactly the same, the mechanism is widely different. An electric force rolls electrons up an electronic gradient that converts ADP to ATP (the top of the electronic hill). ATP is a chemical that stores energy and is sometimes called “the energy currency”. Natural food contains all the ingredients that provide us with fuel. But it also contains vitamins and essential minerals that enable our cells to turn the calorie bearing part of the food into chemical energy. The chemical energy has to be transduced to electrical energy, so the body can be defined as an electrochemical “machine”.
Dr. Marrs and I have long been concerned that concentration on many artificial foods, particularly those concerned with sugar in all its different forms, results in manifestations of disease that are being constantly overlooked and misdiagnosed. We have hypothesized that the symptoms experienced in the early stages of this kind of malnutrition are multitudinous and do not fit into our categories of so-called organic disease. Often attributed to psychosomatic causes, and the prevailing inability to recognize its true underlying mechanisms, has led to frequent doctor shopping by people that have genuine disability. They go from specialist to specialist, all of whom have resolutely decided that vitamin deficiency in America is a thing of the past.
What can you do?
First of all, recognize that dietary mayhem, particularly in children, is common. This results in loss of cellular energy that has its main relevance in the energy consuming brain. Chronic fatigue is perhaps the commonest symptom, but heart palpitations, headache, cold and heat intolerance and other functional symptoms may occur. The peculiarity of behavior observed in someone is because of distorted brain function that can vary enormously in the way it is expressed. I would suggest that if a loved one in his fifties begins to show the signs of aging discussed above, the first thing to do is remove sugar from the diet. Books have been written directing us toward a healthy diet but our pleasure loving brains have become addicted to sweet taste since the earliest beginnings of life. Therefore, because nobody objects to taking pills for their health, appropriate supplements can restore the balance between calories and vitamins. The most under appreciated vitamin (thiamine) may actually be the most important of all of them. However, if we look at the history of the treatment of beriberi, it took huge doses of vitamin B1 (thiamine) for months to restore health. A dose of 100 mg of thiamine hydrochloride, together with a similar dose of magnesium and a multivitamin might be better than all the pharmaceuticals in creation. There is abundant evidence to suggest that neglect of these functional symptoms may gradually lead to biochemical changes that are irreversible and we then call it a neurodegenerative disease.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image credit: Gerd Altmann from Pixabay