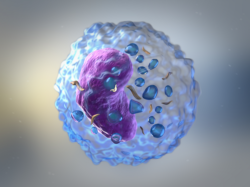
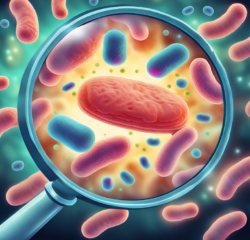
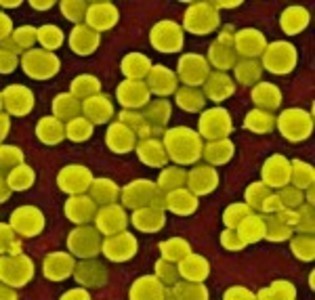
If you are like me, you unnecessarily worry about things completely out of your control like untreatable illness (amongst many other things – from radiation poisoning to earthquakes and of course the zombie apocalypse). As I hear about the increase in antibiotic-resistant diseases, I comfort myself with the fact that I do not use antibacterial products, have not taken an antibiotic in at least five years, and have a super strong immune system (I’ve been sick with the flu once in the last three years and have not had a head cold in the last four to five years). Still, I have an irrational fear of these super-bugs; specifically the flesh eating virus. That’s why I was delighted to read that a new study reveals a treatment that does not involve antibiotics; a treatment that can boost the immune system 1000x’s so the body can fight off these infections. This new study found that vitamin B3, or nicotinamide, taken in large doses was able to kill staphylococcus aureus in both mice and human blood samples. The vitamin B3 significantly boosts the number and effectiveness of neutrophils, or white blood cells that target infections. Various news reports noted that this treatment, unlike antibiotics, won’t kill the natural bacteria in our stomach that are necessary to our immune systems.
It is important to note that the doses used in this study are above the government recommended daily intake of vitamin B3 and should not be attempted through diet, over the counter supplementation or without the supervision of medical professionals.
Click here to read the full report in the Journal of Clinical Investigation
The article was originally published on Hormones Matter in September 2012.