Several years ago, when I just beginning to understand the role of nutrient co-factors in mitochondrial health, I was working with a young woman who had been injured by Gardasil. She was my first ‘case’, contacting me online after a post I wrote about the thyroid damage done by this vaccine. Thyroid damage is among the more common disease processes initiated by many drugs and vaccines. It is one of the easiest problems to rule in or out, but more often than not, it is missed by most practitioners. Inasmuch as thyroid and mitochondrial function are reciprocally connected, where there is damage in one, there is damage in the other, and inasmuch as thiamine is requisite for healthy mitochondria, correcting thiamine deficiency can, in many cases, improve thyroid function. When I first met this woman, I did not yet fully appreciate that connection. Eventually, I would be introduced to Dr. Lonsdale and his work on thiamine deficiency, and so began my education. Together, we wrote a book about the role of thiamine deficiency in mitochondrial illness: Thiamine Deficiency Disease, Dysautonomia and High Calorie Malnutrition.
Exercise and Mitochondrial Healing
Her case is unique for a number of reasons, but mainly because, in addition to the thiamine and other nutrients required to heal, she used, and continues to use, exercise to manage her health. That is what I would like to talk about today: the role of exercise in mitochondrial health. Before we do that, below is a synopsis of her case, as reported in our book on pages 286-87. Her full story was provided on our website here.
In 2008, 26-year-old G.C., a previously healthy, athletic young woman, finishing a Master’s program in finance, received the three injections of the Gardasil vaccine. It bears mentioning that 2 years prior she received several travel-related vaccines including diphtheria, typhoid, yellow fever, hepatitis A and B, the flu vaccine, and a tetanus boost and suffered no apparent ill effects.
After the second injection of Gardasil she experienced a flu-like episode with high fever lasting over a week. Full-blown hypersomnia manifested shortly thereafter and worsened to the point where she was able to sustain wakefulness for only 45 min to a maximum of 3 h per day. She experienced fatigue, muscle weakness, and dizziness. Over the next several months she developed tachycardia, intense salt cravings, with concurrent dizziness and thirst. The salt cravings led to blackouts and as she described “waves of extreme somnolence” that included slurred speech, lack of coordination, and imbalance. She learned to keep salt with her at all times. Both physical (e.g., walking, standing up, cooking) and mental exertion were profoundly draining. She reported that if she became angry or experienced any emotional event, she would immediately fall asleep. Multiple doctors had been seen and tests completed. By 2010, only low levels of vitamin D had been recognized.
Narcolepsy, Hypersomnia and Exercise
In late 2010, the fifth physician seen, it was diagnosed as narcolepsy without cataplexy–hypersomnia. She was prescribed 300 mg per day of Modiodal (Modafinil, Australia; Provigil, United States). Wakefulness increased, but she was still dizzy and required multiple hour naps after any exertion. She returned to working out. By the end of 2010 she began a PhD program and was determined to “power through.” She found that exercise, though difficult, allowed her to avoid blackouts. Of note, cardio-type workouts provided respite from the dizziness for 4–6 h, whereas weightlifting netted 24 h without dizziness. Similarly, she observed that if she ate simple sugars or carbohydrates the dizziness and blackouts would return.
Six months after beginning Modiodal her health continued to decline despite experiencing greater wakefulness. She developed severe noise and light sensitivity, continued to experience dizziness, and required excessive amounts of sleep, sea salt, and water. She developed a thick, dry, painful scale on her scalp. Another series of doctors could offer nothing and suggested the illness was in her head, inferring that she “needed to pull herself together.” Despite her health issues she defended her PhD in July 2013.
By October 2013 she had seen 10 physicians as her health continued to decline. She read our work on post-Gardasil thyroid dysfunction and other adverse reactions and requested additional testing. Hashimoto’s, hypogammaglobulinemia, vitamin B deficiencies, and low potassium levels were identified. On several occasions she attempted to get transketolase testing but was unsuccessful. In Nov. 2013 she decided to treat empirically beginning with 100 mg thiamine tetrahydrofurfuryl disulfide (TTFD). She subsequently developed the paradoxical reactions discussed in Chapter 4, with her symptoms worsening.
The Paradox or Refeeding Syndrome
With the dizziness and increased heart rate she reduced her dose to 50 mg of TTFD. Over the course of the next 5 weeks, the tachycardia landed her in hospital on four occasions. By December 2013 her body adjusted to the dosage of TTFD and the tachycardia and dizziness subsided. This is important to note. Long-term dysfunction of this nature requires new knowledge from the physician. Though not damaging to the patient it is regarded as “side effects” and either the patient or the physician stops the treatment. This effect was known to the ancient Chinese and regarded as examples of yin and yang by acupuncturists.
Over the course of the 5 years of progressively declining health she saw a total of 24 doctors. None of whom was able to identify or treat what was ultimately a metabolic disturbance brought on by thiamine deficiency that was likely triggered by the vaccine. Her final diagnoses included cerebral salt wasting, POTS, beriberi, hypersomnia, and Hashimoto’s. Arguably, the thiamine deficiency and the mitochondrial damage that ensued were at the root of each of these diagnoses.
Maintaining Health Post Gardasil
Since 2013 she has continued to maintain her health with thiamine, magnesium, and a cocktail of other mitochondrial supplements (which included very high doses of coenzyme Q10), along with thyroxine for Hashimoto’s and Modiodal to treat the somnolence. As of this writing she is doing well, training in various Asian forms of kickboxing daily and working full time. Without the balance of heavy training, the cocktail of supplements, the Modiodal, and thyroxine, her symptoms reappear.
Her case is remarkable for a number of reasons. First, that she recovered at all is impressive. Many women injured by Gardasil do not recover. She did and continues to thrive all of these years later. Her recovery was not linear though and her continued health requires aggressive attention. I think this process throws many people. We have been trained to expect that recovery from illness proceeds in a logical, linear, and expeditious manner. It does not. There were many setbacks, including several hospitalizations when she first began supplementing with thiamine. Had she not persisted through these setbacks, she might not have recovered her health. Moreover, had she not recognized the fragility of this recovery and continued to actively manage her health all of these years later, she could have easily become seriously ill again.  Indeed, there have been many relapses over the years, where her health declines significantly and requires extended periods of recovery. Nevertheless, she is able to recover and that is remarkable.
Indeed, there have been many relapses over the years, where her health declines significantly and requires extended periods of recovery. Nevertheless, she is able to recover and that is remarkable.
Secondly, and what I think is particularly unique about her case, is the role that exercise has played in her ability to recover and maintain her health. It is not something that conventional or even functional medicine gives much credence too. Sure, we all recognize the role of exercise in health generally, but mostly, we ignore it. I think this is a mistake. In her case, exercise was and remains critical to maintaining her mitochondrial health and as I have come to understand recently, the type of exercise that she gravitated towards naturally, kickboxing, may be exactly what her brain needs to function.
The Role of Exercise in Recovery
From the beginning of her illness, she forced herself to exercise, even though it was an immense struggle. On her own, she learned that certain types of exercise would prevent her dizziness and blackouts. Specifically, if she did cardio-type exercise, she could prevent a blackout for 6 hours or so, but if she added some weightlifting, the effects would last for up to 24 hours. I attributed this to exercise-induced mitochondrial biogenesis. That is, exercise was forcing the birth of new mitochondria, and somehow, shifting her balance of unhealthy to healthy mitochondria more favorably. It was also likely improving the respiratory capacity of her existing mitochondria. Although it is still not clear to me why one modality yielded better results than another, as the research in this area seems to suggest that the opposite is true, that cardio yields more mitochondrial benefits than weightlifting, the research is clear that exercise induces both mitochondrial biogenesis while improving their functionality.
Her seemingly innate realization of this was and remains one of the more noteworthy aspects of her case. Remember, for several years after Gardasil vaccine, she was seriously ill. When she first contacted me, she weighed less than 100 lbs, was severely fatigued, and could not maintain wakefulness for more than a few hours at a time without blacking out; and yet, somehow, she managed to drag herself to a gym to exercise (and maintain her graduate work in finance). Not only that, she observed a pattern of response to exercise (and salt and other dietary components) and used what she learned to help herself function better. Indeed, throughout her recovery, she would actively observe the patterns and optimize those that appeared beneficial and eliminate those that did not; something that we all should be doing as a matter of course, and yet, very few of us do.
To exercise throughout an illness where intractable fatigue, excessive somnolence and blackouts dominate is very difficult to do, and more often than not, would be discouraged. When I first wrote about her using exercise to heal, the backlash was immediate and intense. For her though, the exercise became an integral component of maintaining her health just as surely as the nutrient elements. Even now, 12 years from initial vaccine-induced illness and with 7 years of recovery under her belt, she indicates that when she misses training because of work or travel, her health declines rapidly and does so in a fairly specific manner. She becomes dizzy, loses balance, and her cognitive capacity diminishes significantly. Her ability to maintain wakefulness declines while fatigue increases. Additionally, when the stress of normal everyday illnesses come into play, a viral infection for example, and her exercise program naturally takes a hit, in order to fully recover she has to double-down on the training for a period of time once the illness passes.
Is this need to exercise unique to her case specifically or could we learn something about how we approach recovery from illness? I would argue that given the mitochondrial fitness attributable to exercise and the noted mitochondrial decline in its absence, some form of movement or exercise should be approached with any recovery plan. If this is the case, the questions become, at what point in the illness or recovery should exercise be considered, how much, and in what form? While the answers to these questions are far too individual to explore fully here, what we learn from her case is that exercise, when implemented early, improves recovery. That brings us to a more complicated question; why kickboxing, boxing, or other dynamically challenging programs might be useful for narcolepsy specifically. From what I have learned, it may be related to activating and training neural connections in a region of the brain called the basal ganglia. And of course, the mitochondria are still involved.
Enter Kickboxing and the Basal Ganglia
I believe there is damage to the basal ganglia for her and other Gardasil injured women. To this point, among the more common symptoms associated with Gardasil injury are tremors, ataxia, and gait issues. While those symptoms can easily be attributed to cerebellar and thyroid damage as well, and both of which are affected by the vaccine and thiamine deficiency, it is not without warrant that we look at the basal ganglia for these symptoms, as well as for the sleep and wakefulness issues. Neural tracts between the cerebellum and basal ganglia suggest that if one is damaged, messaging and functioning to the other would be impaired. Indeed, research shows both efferent and afferent disynaptic (from and too, two neuron) connections between the cerebellum and the basal ganglia. Additionally, personal communications with other women affected by Gardasil regarding imaging results confirm damage to the basal ganglia in some women. This is in addition to potential cerebellar damage.
Symptomatically, many post-Gardasil women display an ataxic, drunken sailor like gait, which is indicative of cerebellar involvement while their tremors occur at rest, along with muscle rigidity and dystonia, indicating basal ganglia involvement. All of them suffer from what could be termed hypersomnia and excessive fatigue, but none that I have met thus far were diagnosed with narcolepsy, like this patient. Of course, that does not exclude the possibility that it does not exist. The post vaccination symptoms are diverse as one might expect with mitochondrial damage and autonomic system dysfunction.
Why the Basal Ganglia?
The basal ganglia are set of nuclei buried deep in the brain that are responsible for controlling movement, motor learning, executive function (via connections with the frontal cortex) and emotional regulation and motivation (via connection to the limbic system). See figure 1.
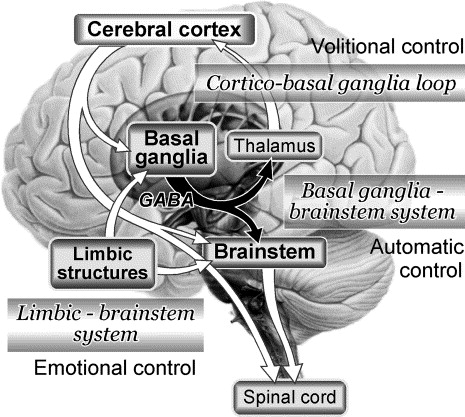
The basal ganglia act as a breaking system to complex movement patterns and activities.
The most well known disorders of these nuclei include Parkinson’s and Huntington’s diseases. These are dis-inhibition syndromes, where the normal inhibitory control that the basal ganglia hold over motor movements is lost resulting in tremors and chorea respectively. There are also problems with initiating movement. This occurs via connections to the limbic system, particularly a set of nuclei located in what is called the ventral tegmental area (VTA). These nuclei are central to motivating behavior, addictive behavior in many cases, but also, behavior in general. The dopamine released by the VTA neurons provide reward and reward, as we all know, encourages habit and learning. That hit of dopamine gives us the drive to act. As Parkinson’s disease progresses, patients lose these connections and with them that internal, unconscious motivation that initiates behavior. They become stuck and so absent an external cue, patients will become unable initiate a movement internally on their own. This stuckness might sometimes also manifests as a sort of depression; one where there is no motivation to act at all.
One of the latest alternative treatment modalities for Parkinson’s disease, aside from thiamine, involves boxing. Yes, boxing. Boxing, because of the balance requirements, the bilateral, stop/go and cognitively active nature of the exercise seems to activate tracts in the basal ganglia that increase inhibitory control, reduce tremors, and allow for a smoother initiation of movement patterns. It also improves gait speed and balance, conditioning, cognitive ability, and overall quality of life.
What does all of this have to do with the ability to maintain wakefulness, and as our patient indicated, cognitive clarity? This, as far as I can tell, has not been studied, but I suspect it has to do with enhancing motivation. Not motivation in the psychobabble sense, but motivation as a fundamentally physiological, survival-based behavior; motivation that is controlled by the basal ganglia via connections to the limbic system and the frontal cortex, respectively. That hit of dopamine that engenders motivation is key for not only movement but arousal. When there is damage to that system, wakefulness is near impossible. Rodent studies have born this out. Without ‘motivation’ we cannot remain awake and we cannot sustain the arousal necessary for mental acuity.
Consider for a moment, the key aspect among all of the behaviors controlled by basal ganglia is that they necessitate wakefulness. Given that, it makes sense from a purely logical perspective that the basal ganglia might be involved in maintaining the arousal necessary to perform these activities. Similarly, it makes sense that damage to certain tracts within these nuclei could impair not only one’s ability to maintain wakefulness, but also, one’s ability to manage motor movement with altered sleep/wakefulness patterns. Finally, absent sustained and vigilant wakefulness, mental acuity is impossible. The cognitive fogginess, so often reported by these patients, may very well be linked to disruptions in basal ganglia functioning.
But Wait, There is More: The Orexin System and the Basal Ganglia
When narcolepsy and other sleep/wake disorders are researched, the basal ganglia have only recently come into view. This is despite the fact that the most well-known disorders of the basal ganglia, like Parkinson’s, demonstrate clear sleep/wake disturbances. Instead, another set of neurons located in the hypothalamus, called the orexin/hypocretin neurons (same neurons, different name), dominate the research landscape. Damage to these neurons is clearly linked to narcolepsy, cataplexy and other sleep/wake disturbances, and for our purposes, directly attributable vaccine reactions, especially the flu vaccine. The basal ganglia, not so much. How do we reconcile the known connections between orexin system, narcolepsy, and vaccine damage, the paucity of research on the basal ganglia. Well, like everything in the brain and body, we look for communication patterns. And it just so happens, the orexin neurons clearly interact with the basal ganglia to manage arousal, both directly via orexin receptors in various regions of the basal ganglia and indirectly, via vast projections throughout the limbic system, which then project to the basal ganglia.
Backing up just a bit, the release of orexin induces wakefulness. I have written about this system here, here, here, and here. When orexin neurons are turned on and firing appropriately, arousal is maintained. When orexin neurons are turned off, diminished or dysfunctional, melatonin, the sleep promoting hormone, is turned on. The two work in concert to manage wakefulness and sleep. Orexin receptors are located throughout the central nervous system and in the body. For our purposes, the orexin receptors in the amygdala and throughout the limbic system directly activate the release of dopamine from the VTA. Recall, dopamine projections from the VTA to the basal ganglia are critical for motivating and sustaining wakefulness in Parkinson’s patients. Additionally, orexin receptors have been found in different regions of the basal ganglia themselves, suggesting direct regulation of arousal. Perhaps even more importantly, the orexin neurons have been found to be instrumental in integrating motor movement patterns.
“…numerous neuroanatomical and immunohistochemical studies reveal that essential subcortical motor structures, such as the basal ganglia, cerebellum, and vestibular nucleus, receive direct innervation from orexin neurons. Moreover, during movements, orexinergic neurons are particularly active and orexin release increases. The evidence suggests that the orexinergic system directly participates in central motor control.”
So what we have is an integrated system of arousal, movement control, and cognitive behaviors that relies heavily on the health and functioning of the basal ganglia and its connections through out the brain, including with orexin system in the hypothalamus. And the orexin system itself relies heavily on functioning mitochondria, as does everything, but the orexin neurons are particularly sensitive to diminished mitochondrial function as these neurons require as much as 5-6X the amount of intracellular ATP to maintain firing compared to other neurons. The orexin neurons cease firing when ATP stores become low, inducing sleep to allow the reallocation energy towards more basic survival functions like heart rate and respiration. That means that excessive sleep is to be expected with mitochondrial damage.
Putting It All Together
With direct stress to the mitochondria via vaccines and medications we can expect a variety of negative symptoms. In this case, our patient developed thyroid damage, autonomic dysfunction (cerebellar and brainstem involvement), and likely also, some degree of basal ganglia injury. The hypersomnia, so commonly experienced during illness or adverse medication/vaccine reactions, represents diminished orexin activity likely initiated by diminished mitochondrial capacity. Narcolepsy suggests a specific injury to oxexin system. With the diminished orexin capacity, we can anticipate that basal ganglia function would be impacted, and with it, the ability to maintain the requisite ‘motivation’ for arousal and wakefulness and to coordinate movement and maintain cognitive acuity. Nutrients and exercise improve the respiratory capacity of mitochondria, which in turn, provides the requisite energy to manage autonomic function from the brainstem and cerebellum and to sustain wakefulness by maintaining orexin firing in general and to the basal ganglia more specifically. Additionally, exercise that demands dynamic, bilateral, complex movement patterns, such as kickboxing, may serve to retrain or maintain the strength of synaptic connections to, through, and from the basal ganglia, which ultimately, may offset any damage done by the initial insult.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on March 12, 2020.