The hysterectomy and oophorectomy industry continues to flourish. There are over 600,000 hysterectomies every year. The oophorectomy rate is about 70% of the hysterectomy rate, some performed at the time of hysterectomy and others as separate surgeries. About 90% of these surgeries are for benign conditions (elective). These are merely estimates based on samples of inpatient data from short-term, acute-care, nonfederal hospitals along with hysterectomy and oophorectomy outpatient percentage estimates. According to the aforementioned publication, the rate of outpatient (ambulatory) hysterectomies increased from 14% in 2000 to 70% in 2014. Outpatient oophorectomies increased from 57% to 84% over the same time period. The Centers for Disease Control (CDC) reports only inpatient hysterectomies which is why hysterectomy rates are typically understated by the media. A 70% understatement is a gross misrepresentation and outpatient hysterectomies may now exceed 70%.
Hysterectomy is seen as panacea for a multitude of women’s health issues. Unfortunately, it is not, and yet, this perception that hysterectomy is a cure-all survives, largely because of false information from gynecologists, gynecologic oncologists, other medical professionals, hospitals, surgical centers, the media, and women who have had the surgery(ies).
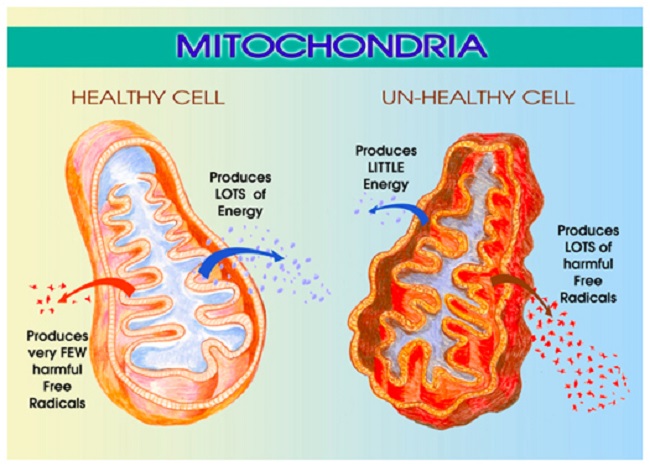
The prevalence of hysterectomy and oophorectomy leads the public to mistakenly believe that a woman’s sex organs are disposable. In many cases, gynecologists fail to provide their patients with the necessary factual information to make an informed decision about these surgeries, leaving women and their partners to learn about the side effects after the fact. Some of the more commonly reported side effects include: bladder and bowel dysfunction, skeletal and figure changes, sexual dysfunction, emotional emptiness, and impaired ovarian function. Although some may believe these side effects are rare and thus rarely discussed pre-surgery, comments on these hysterectomy articles indicate they must be more common than many realize.
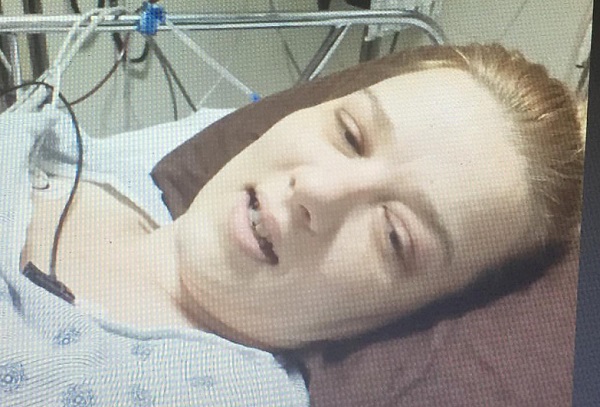
What makes these side effects even more troubling, is the fact these procedures are rarely needed. Women are coaxed into the surgery under the false pretense of cancer or pre-cancer or told it is their only or best option. Finally, many women’s organ(s) are removed despite having specifically told their surgeons that organ(s) should not be removed. Here is just one of those stories.
In light of the problems with hysterectomy, the HERS Foundation is collecting stories of post-hysterectomy problems. We are supporting that effort. If you would like to share your story, consider participating in the “In My Own Voice” project. To learn more, click here.
If you would like to share your story here on Hormones Matter, please contact us here.
Thank you in advance for sharing your hysterectomy experience.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.