I was first diagnosed with severe osteoporosis when I was thirteen years old. I am now thirty three. My osteoporosis was secondary to prolonged malnutrition, delayed development and low weight caused by severe gut complications stemming from Ehlers Danlos Syndrome (EDS) – a heritable connective tissue that runs in my family. Osteoporosis can be a very challenging disease to treat, as bone is incredibly slow to rebuild.
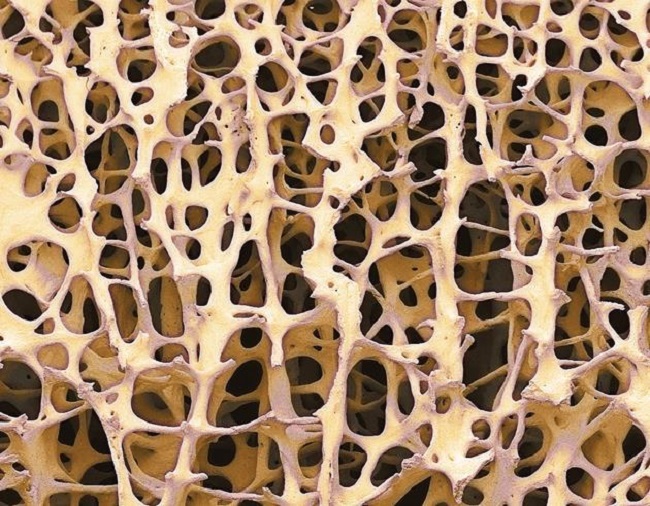
It’s hard to describe the fear associated with having osteoporosis at any age – the sense of porosity in the structure holding you together, the deep dread of your fragility holding you back from participating fully in life, the terror that you could sustain a serious fracture, which among the elderly, could be fatal.
Living with osteoporosis constantly challenged my confidence. I couldn’t help internalize the feelings of failure and weakness for having bones more fragile and brittle than someone nearing the end of their life, let alone just beginning it. Subsequent bone injuries from exercise (including hip stress fractures and shin splints) were a constant source of both pain and stress.
For years following my diagnosis, I had no clear way to treat the illness, as the causes of my debilitating gut issues and low weight remained a mystery, until my early twenties when I was diagnosed with EDS.
I remember the first time I had a DEXA (bone density) scan following my EDS diagnosis. The osteoporosis had gotten worse, not better. The junior doctor allocated to discuss my results could not contain their shock and had to leave the room at one point. My spine was particularly bad with a T score of -4.5. For context on what this means:
- Normal: 0 to -1
- Osteopenia: -1 to -2.5
- Osteoporosis: -2.5 or lower
- Severe osteoporosis: -3.5 or lower
I felt overwhelmed navigating all of the literature on how best to treat osteoporosis. And I struggled to overcome the terror instilled in me from looking at too many photos of brittle, hollow bones. I couldn’t help feeling awfully hollow inside.
Given the severity of my condition, I was encouraged to take bisphosphonates – a class of drugs that slow down bone loss. However, researching the side-effects (which include bone and joint pain, jaw problems, gut and kidney issues), I decided against this. Considering what I stood to lose by not treating the osteoporosis, this was not a decision that I took lightly.
Instead, I pored through journal articles, books and videos, eventually cobbling together a plan of action that integrated nutrition and exercise to heal my bones.
It’s important to mention here that I consider treating bone health just one part of treating overall health. My overall health was very compromised, so I had to take a holistic approach.
Treating my severe gut issues was my first priority. My gut was so dysfunctional that it regularly became impacted and was often silent on ultrasounds, indicating little to no movement was taking place. I often ended up in hospital in agonizing intestinal pain from all the pockets of air that would form around the sites of impaction. I began taking an entero-kinetic medication to help restore peristalsis to my gut. This enabled food to move through and nutrition to be absorbed. It also helped me to increase my food intake.
My gut flora was really compromised from years of malnutrition and dysmotility, so I also began a course of herbal therapy. The herbs were originally prescribed to treat another condition I was dealing with (chronic neurological Lyme disease), however they also ended up massively improving my gut. I know this because prior to starting the herbs, I suffered from multiple food intolerances and major FODMAP issues. After taking herbs for eighteen months, all of my gut problems subsided and I can now eat all foods with no discomfort, including dairy products which I have struggled with all of my life. This made getting adequate calcium from my diet a lot easier than simply relying on supplements. The herbs I used are those prescribed for Lyme disease by American herbalist Stephen Buhner, and adapted by Dr. Bill Rawls. You can see specific ingredients at Dr. Rawls’ website by searching (see Advanced Biotic and Adaptogen Recovery).
Fixing up my gut allowed me to eat from a wide range of foods, but critically it enabled me to restore my weight to a healthy level. I was underweight from the ages of thirteen to thirty, which led to primary amenorrhea. Restoring my weight and menstrual cycles played a vital role in helping protect my bones. Low weight is the most common cause of hypothalamic amenorrhea, and this lack of periods leads to estrogen deficiency which adversely affects peak bone mass and increases the risk of osteoporosis.
I follow a healthy whole foods diet, however I am no purist. After years of restrictive diets in the hope of fixing my gut problems, I am now a big believer in non-restrictive approaches to eating. In my experience, scarcity mindsets and restrictive eating rarely does good things for our bodies and minds. So, I now eat from a wide variety of foods, and have no foods which I consider off-limits. I would say my diet primarily comprises fresh fruits and vegetables (several, with plenty of different colors, at every meal), whole grains, legumes, nuts and seeds, goat’s milk yoghurt, avocados, parmesan cheese, seafood (particularly fatty fish like salmon, and sardines), tofu and tempeh, grass-fed whey protein powder, root vegetables, and a little lean meat mainly in the form of kangaroo and chicken.
In addition to restoring my gut health, I added in a range of supplements to strengthen my bones. After researching multivitamins, I settled on the Calton’s Nutreince because it is available as a powder (EDS can make swallowing capsules challenging) and was formulated specifically to treat osteoporosis. You can read more about the multiyear process that the Calton’s went through to develop this product in their book Rebuild Your Bones.
Nutreince contains 500mg of highly absorbable calcium citrate together with Vitamin K1 & K2, Vitamin D3 and other bioavailable micronutrients that are crucial for bone health. I took a little extra Vitamin D on top of that found in Nutreince, to bring my daily intake up to 3000 IU, ditto with calcium to ensure I was getting 1200mg of calcium per day from a combination of food and supplementation. The food sources I relied on for calcium primarily included things like parmesan cheese, goat’s yoghurt, grass-fed whey protein powder, salmon with the bones, sardines, and to a lesser extent nuts, legumes and leafy green vegetables.
The remaining part of my action plan was exercise. I took up high load strength training, supervised by an exercise physiologist. I train three times per week for an hour each time (including mini rest breaks between sets). My program includes a rotating range of moves, but for the bones particularly – bench presses, deadlifts, and squats. I am currently squatting 45kg, deadlifting 50kg, and bench pressing 30kg. Each week, I aim to increase the weight that I lift, such that I can do 5 reps, with only 2 remaining reps in reserve (i.e. I could only lift that weight another 2 times before running out of strength). For context, I weigh 56kg, so I am gradually moving up to be able to lift more than my body weight. I never imagined myself lifting weights, but the feeling of strength I am building through each successive session is a wonderful experience.
I also removed some things. These included: long distance running – which, in my case, was stimulating excess cortisol and increasing my rate of injury. Given my history of gut issues, I tend to find it hard to fuel this level of endurance exercise (I used to run half marathons), which in turn sets me up for a higher risk of lower bone density. In time, this may shift, but for now, I am sticking to shorter distances and thinking of resuming soccer, given its fun and research shows it contributes to strong bone density. Bones get strong when they are loaded from multiple directions, hence sports like soccer are great, compared to things like long distance running which involve moving only in one direction for a long time.
I also worked on reducing my overall stress levels. I was a chronic workaholic, so (not without difficulty) I reduced my work hours, took up meditation and started therapy. I also gave up coffee, given research linking caffeine and bone loss. I have never drunk alcohol, which when consumed regularly and in large amounts, can also increase the risk of low bone density. However these choices are personal only, and coffee and alcohol in moderation, may not be a problem for some.
So in summary, this is what I did:
- Healed my gut and overcame my food intolerances with herbal therapy
- Increased my food intake (from a wide, unrestricted range of whole foods) to restore my weight and menstrual cycle
- Ensured intake of key nutrients needed for bone – from both supplementation and diet – equivalent to 1200mg calcium, 3000 IU of Vitamin D and at least 120mcg of Vitamin K1 & K2
- Added in supervised strength training 3x per week building to being able to lift more than my own body weight
So, how did all of this stack up? The proof is in the results. Below is a summary of my T scores over the past four years.
A few things to note before you read these results:
- Bone can take up to nine years to remodel, so these results are showing you only partial results of the changes I’ve primarily made in the past three years
- These results have been achieved since turning thirty, which is the age at which peak bone mass is achieved.
- Regarding the hip scores – the 2022 measurements were done using a more sensitive measurement technology called QCT, as opposed to DEXA technology used in previous measurements. QCT consistently produces lower scores than DEXA, so is not a fair comparison with the 2020 and 2018 scores. If these were DEXA scores, they would likely be higher, i.e. show greater improvement.
| 2022 | 2020 | 2018 | |
| Spine | -1.1 | -3.6 | -4.2 |
| Femoral neck | -1.59 | -1.8 | -2.3 |
| Total hip | -2.13 | -1.7 | -2.4 |
You should always seek your own medical advice when treating something as complex and serious as osteoporosis, however these results show that it is entirely possible to reverse osteoporosis through nutrition and exercise, without having to endure the side effects of conventional pharmacological treatments, nor the ongoing fears that living with the prospect of an incurable disease too often instills.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on June 1, 2022.