In a previous article, I discussed some of the many possible causes of female sexual pain. In this follow-up I will discuss how physical therapy can address some sources of pain with sex, give guidance on how to find a therapist, and offer tips to consider when engaging in this specialized type of physical therapy.
A thorough examination by a gynecologist is always the first step in addressing pelvic pain, as not all causes of pain can be treated with physical therapy. Physical therapy works best to address issues including nerve sensitivity, muscle dysfunction, alignment, fascial mobility, and scar tissue.
How Do You Know If Physical Therapy Can Help You?
Your gynecologist may refer you directly to physical therapy for treatment of your pain. Unfortunately, some physicians are not aware that physical therapy can address these issues, or may not know a therapist that they feel confident sending you to.
Here are some signs that specialized pelvic PT may be able to help you:
- The gynecologist has not found any medical issues causing your pain. If you have visited your doctor, had a thorough evaluation, and have not had any medical findings, your issues may be musculoskeletal. In that case, evaluation by a pelvic PT is warranted.
- Issues with urination or defecation. For example, delayed or incomplete urination, pain with bowel movements or urination, urinary frequency, or urinary leaking may indicate pelvic floor dysfunction.
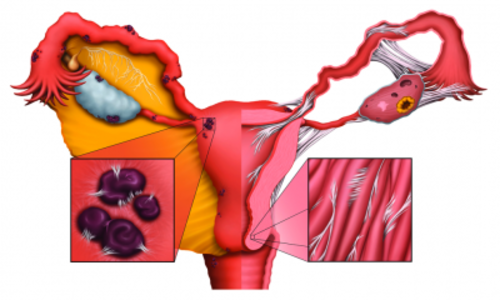
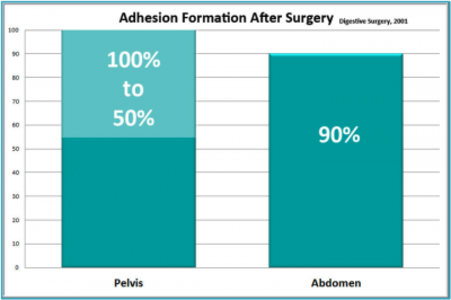
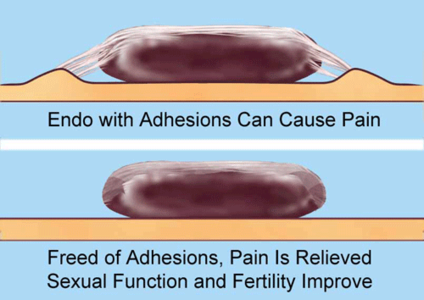
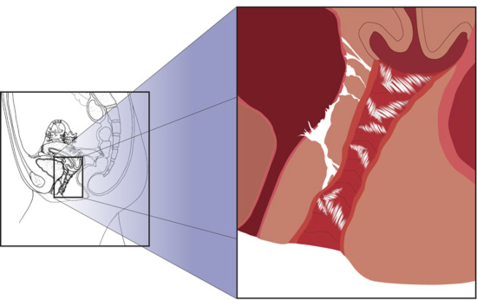
- You have a history of chronic infections, inflammation, or physical trauma. These can cause restriction of the connective tissue in and around the pelvis and pelvic floor. This restriction, over time, builds up and can limit mobility or put strain on pain sensitive structures. Examples might be chronic yeast infections, endometriosis, falls to the tailbone, or sexual trauma.
- You have a history of surgeries or scar tissue. Scar tissue restricts the normal mobility of tissues and puts pressure on pain sensitive structures. Abdominal or pelvic scar tissue can cause pain at the site of the visible scar, or in areas that may not seem connected.
- You have other issues such as lower back pain, poor posture, or discomfort in sitting. The pelvis is integral to the function of the rest of the body, and dysfunctions here can lead to problems elsewhere.
What Does Pelvic Physical Therapy Entail?
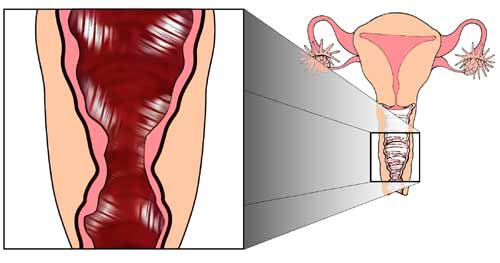
Therapists in this field are specifically trained to treat pelvic structures, both internally (vaginally and rectally) and externally. The most common treatment methods that pelvic health PTs may employ are manual soft tissue work, exercise, biofeedback, and education.
Soft Tissue Work
There are many manual techniques that therapists can use to treat your muscles, joints, connective tissue, and even organs. These each of these techniques requires its’ own specialized training and should not be provided by untrained practitioners. While not a “massage,” these techniques do involve using gentle pressures, applied by hand, to improve function. The most common question I get on this subject is, “will it hurt?” This is an understandable concern – you are going to see the therapist because you have pain, and it can be a scary proposition to have someone touching already painful areas. This is certainly something to discuss with your therapist before treatment so that you are both comfortable with proceeding. In many cases the therapist will need to treat these sensitive areas in order to bring you relief. Because these areas are already irritated you may experience some initial discomfort as the therapist works with them. But the goal of treatment is NEVER to cause pain; in fact this is avoided at all costs. There are strategies that can be used, such as a physician-prescribed lidocaine gel, to make sure you are comfortable.
Exercise
When we think of exercise for pelvic health, most people think of Kegels. However, this is only a small piece of the exercises that can be helpful! Exercises may be prescribed to teach you to relax your pelvic floor, coordinate the pelvic floor with other muscles in your body, or relieve pressure on painful structures by improving posture, stability, or alignment. After evaluating you, your therapist will decide if any exercises are called for in your case. If they are, they will prescribe exercises targeted to improve your specific dysfunctions and will educate you on how to do them safely and effectively.
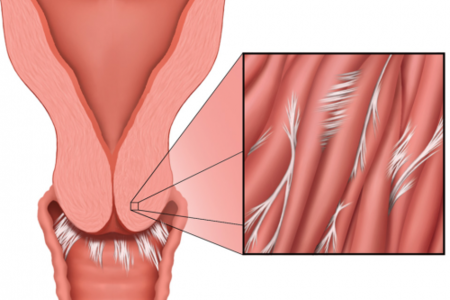
Biofeedback
Biofeedback is any method of giving you feedback on what your body is doing. In pelvic therapy this is commonly done to bring your awareness to your pelvic floor. Using a sensor, the biofeedback machine will determine how active your muscles are and give you a visual cue to help you learn what “relaxed” and “contracted” feels like. This is extremely useful, as many women who have pain with intercourse have muscles that have forgotten how to “relax.” They may be constantly contracted, tight, and painful. Sensors can be used internally (vaginally or rectally) or externally. There are also tools that you can use at home to continue your training outside of therapy.
Education
The primary job of any physical therapist is to educate, and this will begin on day 1 of treatment, with your evaluation. Your therapist will explain to you what s/he is doing and why, and once your evaluation is complete the results should be explained to you. From there you and your therapist will create a plan for your care. You may be educated sexual positions that might be more comfortable for you, lubricants, better toileting habits, sitting and standing postures to reduce stress on the pelvic floor, home treatments or exercises, relaxation techniques, breathing techniques, common irritants to the pelvic floor, and things to avoid as your treatment progresses. I have found that the more educated and informed my patients are, the better their outcomes tend to be! Your physical therapist can be both therapist and coach to better help you reach your goals.
So how do you go about finding a specialized pelvic therapist who can treat your pain? Your primary care doctor or gynecologist may have someone that they refer patients to on a regular basis.
If they do not, you can Internet search your city with the phrases “pelvic floor therapist,” or “women’s health therapist.” Other key phrases to help you narrow your results include “dyspareunia” (pain with intercourse) and “pelvic pain.”
You can also access directories of practitioners. For example, https://hermanwallace.com/practitioner-directory and http://www.womenshealthapta.org/pt-locator/. Therapists listed on these sites have taken continuing education courses in pelvic floor physical therapy. Be aware that not all therapists list themselves on these sites, as some require hefty membership fees to join.
Lastly, here are some helpful tips to consider when beginning pelvic physical therapy:
- Research your therapist. Not all therapists who work with the pelvis may have experience working with your particular issue. It’s okay to research the therapist online, or call them to discuss their background and training.
- Ask Questions. During your evaluation and subsequent treatment, ask any questions that come to you. When you get home, make a list of any questions or concerns that come up, and bring the list to your next session. The more educated you are on your body and treatment, the more comfortable you will be and the more productive your sessions can be.
- Communicate. During treatment please speak up if you are uncomfortable or have pain. We, as therapists, rely upon you for feedback. As I like to say, you are the only person feeling what you are feeling! Please do communicate during and after your sessions so that we can better help you.
- You are in charge. You will be asked for your consent to treatment before any treatment is undertaken. You can consent to all treatment, some portions of treatment, or none at all. You can also decline treatment at ANY point in a session, for any reason. Lastly, you can ask to have someone else in the room while you are treated. You are always in control of your treatment session.
- Keep a Journal. Keeping a journal of your symptoms may help you to track your progress over time. It can also give valuable information if you have a significant change and we are trying to understand the cause.
- Be Proactive. If your therapist gives you a home exercise or self-treatment plan, do your best to work with it. And if they haven’t given you one, it’s okay to ask for it. I find that the more engaged patients are with treatment, the better their outcomes tend to be.
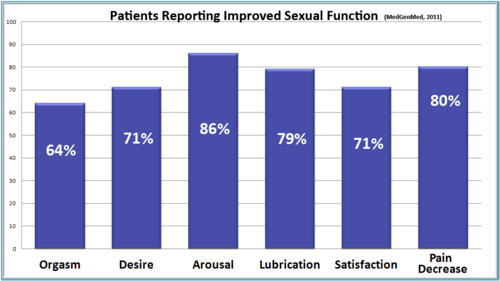
Female sexual pain is more common than most people realize, and in many cases can be treated successfully with physical therapy. Please do not doubt yourself if you are experiencing this- you deserve to have full function, without pain, and it is worth your while to investigate treatment options.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This post was published originally on Hormones Matter on February 18, 2016.