In the current public discussion about autism, one could easily conclude that autism must be caused by either genetic mutations or vaccines. The media, besides portraying these positions as the only two possibilities, typically go even further by portraying them as mutually exclusive possibilities. This kind of distorted presentation crowds out discussion of other causation ideas.
Over the last 10 years I’ve developed my own theory of autism causation, a set of interconnecting biological mechanisms that, taken together, provide viable explanations for a substantial amount of autism data from multiple research areas. In summary, I am convinced that broad and indiscriminate folic acid supplementation practice has caused two concurrent and overlapping autism epidemics in certain susceptible subgroups of the population.
Part I: Early Pregnancy and Neural Tube Formation
The neural tube is the first well-defined structure of the fetal central nervous system, and it is formed by embryonic day 28. It was shown in 1980 that taking folic acid prior to conception and during the first few weeks of pregnancy prevented birth defects of the brain, spine, and spinal cord caused by the neural tube’s failure to close completely (called neural tube defects, or NTDs). In 1992, the U.S. Public Health Service recommended that all women capable of becoming pregnant consume 400 micrograms of folic acid per day, and in 1998, a folic acid food fortification program was implemented. It is estimated that about 1,300 NTD cases per year are avoided in the U.S. due to these measures.
More than 30 years after the initial groundbreaking NTD study, it was reported that prenatal folic acid supplementation was also associated with reduced risk of autism. One study found that folic acid reduced autism risk when it was taken during the first month of pregnancy, and another study confirmed folic acid’s early pregnancy protective effect, but found that it did not extend to mid-pregnancy. The results of these studies are fascinatingly counter-intuitive, given that both autism rates and prenatal folic acid uptake increased during the same time period. If folic acid does prevent autism, then it is puzzling that autism rates fail to track NTD rates; in other words, we would have expected to see a tremendous reduction in autism rates – certainly not the increase in autism rates that did occur – after the U.S. Public Health Service issued its recommendation and folic acid food fortification was implemented in the 1990s. This implies, at the very least, that folic acid’s relationship with autism is not as straightforward as it is with NTDs.
One extremely critical point is that most women in the U.S. are now supplementing with folic acid throughout pregnancy, despite the neural tube’s closure by embryonic day 28. Since there are plenty of substances – alcohol, rubella virus, and thalidomide, to name some better known examples – that have dramatically different effects on a fetus depending on when the exposure occurs, it’s not unreasonable to suppose that folic acid might have different potential effects on a fetus depending on the gestational period of exposure. Folic acid has extraordinary properties, and should not be dismissed as “just a vitamin.”
Part II: Mid Pregnancy and Neurogenesis
A Brief Summary of Normal Brain Development
In humans, neuron production begins on embryonic day 42, two weeks after neural tube closure, and is largely complete by mid pregnancy. Neurons form in a layer of tissue called the ventricular zone, and migrate away to form the brain’s structures and neural networks. The largest processing networks involve the neocortex, the layer of cells on the brain’s surface, and the subcortical nuclei, which lie underneath the neocortex and relay information to and from the neocortex. After migration, cortical neurons undergo extensive structural changes to form the pathways of the brain’s neural networks. They extend long fibers called axons to connect with other neurons, and grow arrays of fibers called dendrites for receipt of electrochemical information from other neurons.
Brain development depends upon complex cascades of molecular signaling involving many genes and gene products. The integrity of the entire process depends on the right elements appearing at the right times and in the right amounts, such that one genetic disruption can impact the entire downstream course of development.
Gene-disrupting mutations are not the only way that the molecular products of genes can be altered; disruptive epigenetic alteration of gene expression can also cause the normal cascade of developmental events to veer off course. Epigenetics is the molecular alteration of a gene’s expression without changing the underlying DNA sequence. These alterations to genes are usually heritable through cell division, although perhaps not from one generation to the next. The most widely understood way that epigenetic change can occur is via DNA methylation, where a methyl group forms a bond with cytosine in the DNA sequence, typically at a point in the sequence where cytosine is followed by guanine, called a CpG site. CpG islands are DNA regions with a high frequency of CpG sites; and hypermethylation of CpG islands, especially in promoter and enhancer regions, is highly correlated with silencing of the associated gene. In other words, too much methylation can render a gene just as nonfunctional as a disruptive mutation can.
Brain Development in Autism
A key factor in the widespread rejection of a causal link between vaccines and autism is the weight of evidence showing that autism is associated with a fundamental disruption in prenatal brain development.
Structural indicators of a disruption in brain development are very common in autism. These indicators include dysgeneses, heterotopias, altered cell morphologies, impairments in synapse formation and synapse plasticity, microcephaly, and macrocephaly. Studies have also found increased numbers of neurons in the prefrontal cortex and abnormal positioning of cortical projection neurons in subjects with autism, which suggests a disruption in neurogenesis between gestational weeks 7-20.
Researchers think that nearly one thousand genes may be involved in autism, with some of the most strongly autism-associated genes being those that are involved in neurodevelopment, synapse formation, and epigenetic functions. In fact, recent estimates suggest that 88% of high-risk autism genes are integral to early stages of brain development, regulating neurogenesis and early neuroblast differentiation, and that 80% of these genes also influence later stages of neurodevelopment such as synapse formation. It has been suggested that this strong association of autism with genes that impact multiple stages of brain development may indicate that autism occurs when the number and nature of gene-disrupting mutations involved in neurodevelopment reach a critical threshold of cumulative impairment in neural connectivity.
Beyond genetics, there is ample evidence that atypical epigenetic activity is also involved in autism. Post-mortem analyses show that tissues from certain regions of the brain are differentially methylated in autism, to the point that researchers have called these differences “profoundly distinctive” as compared to controls and have suggested that autism may be generally associated with a disruption to methylation-associated neurodevelopment. Specific genes found to be differentially methylated in autism include oxytocin receptor (OXTR), glutamate decarboxylase 1 (GAD1), Engrailed-2 (EN2), Reelin (RELN), and MECP2, all neurodevelopment-impacting genes, and the autism-associated genetic conditions of Angelman, Fragile X, and Rett Syndromes all involve disrupted epigenetic processes. Particularly fascinating results were obtained in a study of DNA methylation in peripheral tissue, where the subjects were three sets of monozygotic twins. In each twin set, one twin was diagnosed with autism and the other twin had milder autistic features that did not rise to the level of diagnosis. The twins with diagnosed autism had higher methylation levels than either their undiagnosed twins or their unaffected siblings, hinting at the presence of some environmental factor that increases both methylation activity and autism risk.
As noted above, hypermethylation is typically associated with gene silencing, and gene silencing can affect the entire downstream course of development. So what could cause a derailment of fetuses’ normal methylation activity, causing gene silencing during critical periods of brain development on a population-wide scale?
The answer to that question may lie in prenatal vitamins.
Bathing the Fetal Brain in Methyl Groups
The B vitamin folate is an extremely critical source of methyl group donors for DNA methylation, and folic acid is the synthetic version of folate. Standard obstetric protocol now recommends folic acid supplementation through the entire nine months of pregnancy, which means that the majority of pregnant women in the U.S. are consuming historically unprecedented amounts of methyl groups between gestational weeks 7 and 20, just when fetal genes are causing neurons to form, migrate, and differentiate.
It is known that dietary consumption of methyl groups impacts DNA methylation and gene expression. In animals, it is well established that administering folic acid to pregnant mice alters genetic expression in their offspring. In humans, researchers have found that maternal use of folic acid increases methylation in young children, whereas maternal low folate status is associated with both NTD and hypomethylation in the fetal brain. In sum, current research suggests that “in the rapid period of cell division occurring during fetal development, the level of methyl donors can have a significant impact on transcriptional activity that is maintained into adulthood.”
To explore possible effects of folic acid during mid-pregnancy, we can engage in a thought experiment based on the fairly noncontroversial idea that autism results from the cumulative effect of multiple genetic mutations impacting neurodevelopment. In particular, let’s consider a fetus with some genetic mutations that impact brain development, but with a cumulative effect still below the threshold of impaired neural connectivity that would cause autism. What happens if his mother takes folic acid throughout the neurogenesis period? And what if the fetus also has a common genetic impairment in folate metabolism, perhaps causing folic acid to accumulate in the womb? One possible progression of events might develop as follows:
- The mutated genes cause some errors in brain development.
- Because of the fetus’s impaired folate metabolism, excess folic acid accumulates and causes abnormally high methylation activity during brain development. This causes some unmutated genes to become hypermethylated, which renders these genes essentially non-functional. More developmental errors occur because of this gene shut-off.
- Downstream brain development is altered by both the mutations and the inactivated genes. Hypomethylation of certain downstream genes could be a possibility, if either the mutated genes or the inactivated genes functioned to create molecules involved in epigenetic processes.
- The autism threshold is reached as neural connectivity becomes severely impaired by both genetic and epigenetic malfunctioning. Perhaps neither the genetic mutations nor the hypermethylation would have been sufficient to cause autism in isolation, but in combination they do.
If the above sequence of events were to occur on a population-wide level, it might (a) cause an overall rise in autism rates in supplemented populations, and (b) lead to a finding that genetic mutations involving brain development are particularly common in autism, because the presence of these mutations in utero would put a fetus closer to the autism threshold than a fetus without such mutations.
In fact, children with autism do present with significantly more de novo, gene-disrupting mutations than their unaffected siblings.
Part III: Mid Pregnancy and Estrogen
In mammals, male fetuses go through a period of development where fetal testosterone enters the developing brain, converts to estradiol (an estrogen), and stimulates neuronal estrogen receptors. This period of development, called sexual differentiation, essentially masculinizes the male brain. In humans, it is thought that fetuses are sensitive to estrogen-sensitive brain growth in mid-gestation.
In 2011, I published a paper describing, I believe for the first time, the large overlap between estrogen-sensitive cognitive functions and functions impacted in autism, including anxiety, motor deficits, stereotyped and repetitive movements, epilepsy, hyperactivity and attention deficit, disrupted pain recognition, deranged serotonin system, atypical memory function pattern, and atypical visual-spatial information processing. If we speculate that some form of autism results from excessive estrogen-sensitive brain growth, then male fetuses, with their generally higher baseline level of such growth, would logically be more susceptible than females to this form of autism. This could explain the high ratio of boys to girls in autism.
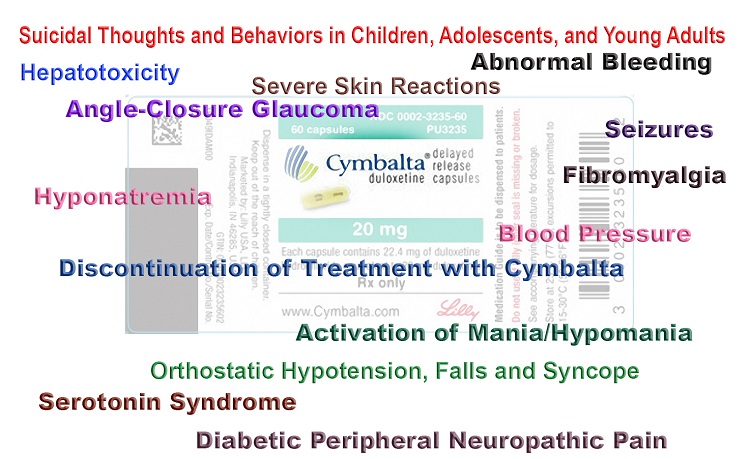
In my article for Hormones Matter last year, I described autism-linked environmental factors that are also linked to estrogenic effects, including hypothyroidism, which is associated with breast cancer; high levels of fetal testosterone, which is relevant because high levels of testosterone would be expected to lead to increased estradiol synthesis; exposure to pyrethroid insecticides, which are known to be estrogenic; maternal usage of selective serotonin reuptake inhibitors (SSRIs), a type of antidepressant that has also been found to be estrogenic; and maternal vitamin D deficiency, a condition also associated with increased risk of breast cancer.
Folic acid is known to stimulate estrogen-sensitive growth in mammals when in the presence of estrogenic substances. It may therefore be the case that excessive quantities of folic acid in the womb during mid-pregnancy, coupled with an estrogenic exposure, is a second path to autism.
Part IV: Two Autisms
Notably, the SSRI and pyrethroid insecticide studies referenced above both found that third trimester exposures were associated with autism. This is well after most neurogenesis is complete. I would suggest that this may demonstrate two distinct risk periods for autism, perhaps even corresponding to two different, yet frequently overlapping, types of autism.
We can imagine that both male and female fetuses with neurodevelopmental genetic mutations might be at greatest risk for hypermethylation-induced autism during neurogenesis. We can also imagine that males with prenatal exposure to estrogenic substances might be at greatest risk for estrogen-induced autism in later pregnancy. The first group might be at greater risk of falling on the low functioning, severe end of the autism spectrum, given the fundamental alteration to brain architecture, whereas the latter group might be more likely to develop a type of high-functioning autism. Accordingly, we’d predict that the ratio of hypermethylation-induced cases to estrogen-induced cases would be markedly higher in females, such that females with autism would be predicted to generally present with more gene-disrupting de novo mutations than males with autism. In fact, this is consistently reported.
Common mutations causing impairment in folate metabolism would be predicted to increase risk for both hypermethylation-induced and estrogen-induced autism. We don’t typically test for these kinds of mutations in fetuses or pregnant women, however, so by the end of pregnancy some fetuses might be swimming in retained folic acid. Up until recently this was not thought possible, but in 2016, researchers from Johns Hopkins found that it was. Moreover, this study found that mothers who retained very large amounts of both folic acid and vitamin B12 in their bloodstreams shortly after birth were 17.6 times more likely to give birth to a child with autism, suggesting that maternal and/or fetal impairments in the folate cycle (which uses vitamin B12 as a co-factor) may be risk factors for autism in supplemented populations. This is very concerning, given that approximately 60% of the population has some degree of impairment in folate metabolism.
Part V: Vaccines
It is important to emphasize that the theory outlined in this article predicts vaccine reaction to be associated with autism.
As I discussed in my first article for Hormones Matter, the kinds of genetic mutations associated with impairment in folate metabolism are also associated with lowered glutathione levels, oxidative stress, and difficulties in fighting infections, resolving inflammation, and removing toxins like metals from the bloodstream. There would thus be an anticipated correlation between generalized detoxification disability and both types of autism. Moreover, eight studies have demonstrated that autism is associated with disrupted genetic expression (but not genetic mutations) with respect to pathways involving inflammation and immunity. This could perhaps indicate that these pathways are associated with autism only because they are vulnerable to hypermethylation via folic acid, not because they play a role in causation. In any case, the administration of vaccines to a child with disrupted inflammation and immunity pathways may have any number of unknown negative consequences – both in the womb and after birth.
Part VI: Conclusion
Folic acid appears to be critical to the earliest phase of human development, as we can see the effects of insufficient early methylation in terminated fetuses with NTDs, and we’ve learned that early supplementation appears to be protective against autism. After embryonic day 28, however, we’re no longer taking folic acid to prevent NTDs. The neural tube has either closed or failed to close by that point, and the fetus has moved onto new stages of development.
Taking folic acid after embryonic day 42, when neurons start forming, may unnecessarily expose developing fetuses to excessive amounts of methyl groups, in some cases disrupting the delicate genetic machinery that produces the molecular products necessary for normal brain growth. And taking folic acid into late pregnancy may aggravate any negative effects of environmental estrogenic exposures, in a world where environmental estrogens are increasing in quantity at an alarming rate. As a standard operating protocol, then, population-wide folic acid supplementation after neural tube formation seems likely to pose an unnecessary risk, especially to fetuses with extraordinarily common mutations that impact folate metabolism.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image credit: love_K_photos / Flickr; CC 2.0; tinting added.