Pulmonary emboli are notoriously difficult to diagnose clinically, especially in otherwise healthy young women. The early signs include such nondescript symptoms as breathing difficulties, chest or back pain, and fatigue; symptoms that are easily attributable to a host of viral and bacterial infections or other less serious respiratory conditions. As a result, and more often than not, it is not until complete hemodynamic collapse that PE is considered; a point at which survival is significantly less likely. Even then, for young women the prospect of pulmonary emboli is not always on the differential. We saw this repeatedly in our pilot study, the Real Risk Birth Control and Blood Clots study where the prospect of birth control induced blood clots was rarely considered. From a review of records and case stories, blood clots seemed only to be considered after everything else was ruled out. That is, they were near the bottom, if not absolutely last, on the diagnostic differential. When the emboli were in the lungs, this refusal to consider contraceptive induced hyper-coagulation has deadly consequences.
When we consider that the most commonly recognized risk associated with hormonal birth control are blood clots, one cannot help but wonder why birth control-induced blood clots are not automatically ruled out when women present to the ER in crisis, but they are not. Time and time again, the early signs of an imminent crisis were dismissed by healthcare practitioners. Neither the deep vein thrombi that frequently preceded the pulmonary emboli by as much as a month, nor the pulmonary emboli were immediately recognized. And as we reported previously, recognition was equally labored in women who developed cerebral venous thrombi, brain clots, often requiring 2-3 ER visits before the diagnosis is even considered. I am not sure why there is such a total break down in clinical acuity when it comes to birth control-induced blood clots, but by all accounts, there is.
Perhaps our familiarity with these drugs has bred a false sense of safety; one so firmly entrenched that even when faced with evidence to the contrary, when life or death hang in balance, we cannot bring ourselves to acknowledge their risks. Perhaps so strong is our desire and need to have effective birth control options, that we employ a sort of willful ignorance about the risks. Or more cynically, perhaps we have simply been duped by Madmen inspired, pharmaceutical funded half-truths and platitudes.
Whatever the reasons, the patient reports suggest that when confronted with evidence of blood clots, all involved tend to dismiss the possibility until all other causes are ruled out. Physicians especially seem reticent to consider blood clots, forgetting entirely that hormonal birth control hyperactivates blood coagulation cascades in favor of clotting – in all women, not just some women, but in all women. They increase pro-clotting factors by 170% and decrease anti-clotting factors by 20%, a change in hemodynamics that all but guarantees a propensity toward body-wide clotting, especially when other health or lifestyle variables are present. No matter the chemistry, however, when clots happen, we all seem genuinely surprised. If the results of this study show anything, it is that birth control induced blood clots are real and should be ruled out first, not last.
Sudden and Slow: The Two Faces of Pulmonary Emboli
One of the key goals of the Real Risk Birth Control Blood Clots study is to identify early warning signs of clotting. To that end, the women who took the survey were asked to identify the presence and severity of 35 symptoms commonly attributed to blood clots, at a month out, a week out, the day before, and the day of, the crisis. Although we found significant linear trends in the escalating severity of many symptoms across time for the group as a whole, more telling were the patterns that emerged when we divided the groups by diagnosis (DVT, DVT + PE, stroke, etc.). There we see distinct patterns in the type of symptoms as well as the trajectory of expression and severity.
For example, when we look at the patterns of early warning signs of pulmonary emboli, we see two, possibly three, trends emerging. In some women, pulmonary emboli seem to appear suddenly with few if any warning signs. In other women, symptoms either increased over time or waxed and waned (or both), sometimes for months, until reaching an apex of severity. For the latter group, the waxing and waning seemed related to the movement of the clot(s) from the periphery to the lungs. That is, the localized pain, swelling, and temperature changes, either in the legs, pelvis, abdomen, or collarbone regions, would be severe for a week or a month before the event and then dissipate entirely, only to re-emerge as the crushing pain associated with the pulmonary embolism. We will be reporting more details in subsequent articles, but preliminarily, the data and the personal accounts suggest the possibility that PEs may be preventable, if the signs of deep vein thrombosis (DVT) are more readily recognized.
Listed below are descriptions of the events leading up to the crisis reported by women with pulmonary emboli who completed Phase 1 of the Real Risk Birth Control and Blood Clot survey. A similar report was published for women who survived strokes.
Sudden Onset
“my chest hurt to the point I could not lay down or move without excruciating pain” – during the crisis – no symptoms prior.
CS2 reports severe right thigh pain the day of the crisis, as well as moderate chest pain, shortness of breath and fatigue and mild back pain, but nothing before that point. The PE caused low blood pressure. Doctors were unable to detect blood pressure in her right arm.
JR began to experience mild discomfort the day before her crisis. The day of her crisis, she explains, “the symptoms [severe shortness of breath, chest pain, irregular heartbeat, dizziness, blackouts, fatigue, and mild to moderate headache, nausea, difficulty speaking, and stomach pain] worsened as the day went on.” She goes on to say that “right before I passed out and then once when I woke up, it was crushing burning pain and my heart was beating so fast that I couldn’t catch my breath.”
RF’s clots originated in the pelvis and legs and experienced severe pain and swelling in the pelvis the day before her crisis.
Tales of Traveling DVTs
“…right lower calf was swollen and warm to the touch, pain felt like a Charley horse. Chest pain was unbearable. It hurt to breathe and my heart was racing so fast that it hurt.” – per her data, leg pain developed a week before but disappeared; chest and heart pain appeared the day of the crisis; fatigue was moderate to severe from week before.
Twenty year old CS reported moderate to severe right shoulder and chest pain a month before the crisis, along with moderate fatigue from a week out. The day of the crisis, the pain moved to lower chest. She describes the chest pain as: “Every time I took a breath in it felt like a knife was being stabbed into my chest on the right side.” Like so many others, she was sent home from doctor’s office day of crisis only to return to ER that night to discover her right lung was riddled with clots, necrotic in places.
KM had very few symptoms leading up to her PE, except a “sharp pain deep in my calf – I thought I had a badly pulled muscle or strain my Achilles tendon (up high) while jogging. The pain got much worse if I was standing for long periods of time, but got much better if I exercised.” She also reports shortness of breath climbing stairs or when giving a presentation.
ES described her symptoms: “leg pain felt like a bad cramp, almost as the back of the leg had seized up. I thought it was a pulled muscle because I lacked other symptoms. The PE pain was a crushing, hot pain in my chest, worse when breathing in.” Her leg pain began a month prior to the PE, peaked a week before and then dissipated entirely. While the pain from the PE began a week prior to the crisis and escalated.
FH rates all of the symptoms leading up to the crisis as mild, even though some of the symptoms emerged months before. She chalked up her leg pain to occasional muscle cramps and the shortness of breath to sinus issues. It wasn’t until she began blacking out that she suspected something more serious was wrong. She notes on the day of the crisis she was cold and her blood pressure was extremely low.
KG reports that “a month before the clots my toes on the right side got red and swollen and felt throbbing. After working out at the gym had chest pain, shortness of breath, [my] ribs hurt, heavy chest that felt like extreme gas pains.”
KD describes how the pain seemed to move with the clot. “The pain in my left quad felt like an injury. Then when it moved to the ribs, it felt like I had pulled ribs. Then when it moved to the right side, it felt like a kidney stone and only hurt bad when I was lying flat on my back. My leg pain, after the clot had already exploded into my lungs, was like a bad Charley horse. My lungs had clots everywhere.”
SD reports severe leg pain 3-4 weeks before experiencing the difficulty breathing associated with her PE.
Waxing and Waning Symptoms
For 43 year old DW symptoms like dizziness, blackouts, and vomiting had emerged a week prior and then dissipated until the day of the event, when they returned along with severe shortness of breath, chest pain and heart palpitations. She describes the pain as “tight legs, stabbing pain and then collapsed. All happened within 5 minutes.”
For DD the DVT that preceded the pulmonary emboli “felt exactly like a Charley horse. When it lasted more than two days and I started limping, I knew I needed to consult a nurse at the ER.” She too had symptoms that waxed and waned over the month preceding the crisis.
R indicated that she experienced breathing difficulties and chest pain that would wax and wane over the six months prior to her PE diagnosis and that it wasn’t until a few days before the crisis, that it became severe. “On the second night when I tried to sleep, I had severe pain in my upper back and left side of my chest, which started to radiate up to my neck and left shoulder. I experienced more pain in my chest if I tried to inhale deeply.”
Unremitting Fatigue as a Key but Non-Specific Symptom
Uncharacteristic and unremitting fatigue was one of the most consistently reported symptoms across all time points and diagnoses.
LL reports severe fatigue for at a least a month prior to the crisis as the leading symptoms. She notes the fatigue appeared well before the pain. “The fatigue leading up to this was very bad. It was such a struggle to get out of bed or do anything. It was there a good while before the pain.” She also reports restless legs, and “severe stabbing pains in my back” especially when “bending down to pick something up.”
Breathlessness and Speaking Difficulties
As one would anticipate with pulmonary emboli, difficulty breathing was a cardinal symptom of the impending crisis.
Breathing Difficulties
“felt like I had become rapidly, extremely unfit. Could not walk up the stairs in one go. Was struggling to get enough oxygen.”
J believes her symptoms emerged months before the crisis. She reports a “hairball-like cough” for months that was continually diagnosed as allergies. It was persistent and would not respond to allergy medicine. She experienced moderate to severe fatigue for the month leading up to the crisis, along with moderate to severe shortness of breath, irregular heartbeat, heart palpitations, cough, dizziness and nausea.
LT said “chest wall pain two weeks before diagnosis felt like soreness from lifting weights. When the back pain localized to my side and upper back, it felt like I had pulled muscles in those areas. The shortness of breath felt like I was getting out of breath way too easily; walking 30 feet felt like I had been running for half a mile, and slowly climbing the long escalator out of the subway station felt like I was trying to run up the stairs.”
SM experienced severe shortness of breath for at least a month prior to her diagnosis. She says she felt as though “…the middle of my chest was being pressed or squeezed.”
Speaking Difficulties
Many women report difficulty breathing in the months, week and day before the crisis. Speaking, because of the breathing difficulties, becomes increasingly labored.
NB said she would gasp for breath and was “only able to get 1-2 syllables between gasps.” She said she felt like she “had run for her life and just couldn’t catch my breath.”
JZ felt “very winded, even in casual conversations,” but otherwise didn’t report any symptoms.
Conclusion
These and other personal accounts of birth control-induced blood clots suggest that for many women, early signs are present but not recognized. Similarly, blood clots appear to be distributed throughout the body. This is consistent with the fact that hormonal birth control induces systemic changes in hemodynamics. To fully delineate the risks, however, we need more data. If you or someone you know has suffered from a birth control induced blood clot, please consider participating in the study.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on November, 2016. We subsequently lost funding to finish this study. Nevertheless, we are still accepting stories about birth induced blood clots. If you’d like to share your story, send us a note: Write for us. Other stories and articles about birth control and blood clots can be read here.
Photo: autopsy of birth control induced pulmonary emboli in a young woman.









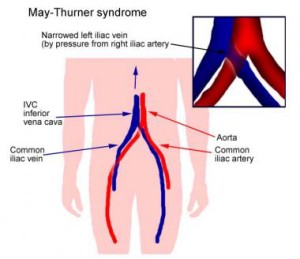 Most do not know this until they end up in the hospital with a blood clot. For these women, the risk for deep vein thrombosis, particularly in the left leg is even higher, especially on birth control (most especially, I believe, though this is pure speculation, when using a cervical ring like the NuvaRing). Again, add long sit times, an injury perhaps, and we can begin to see how the risk for blood clots in the female athlete using hormonal contraception can be much higher than for her teammates who do not use hormonal contraceptives.
Most do not know this until they end up in the hospital with a blood clot. For these women, the risk for deep vein thrombosis, particularly in the left leg is even higher, especially on birth control (most especially, I believe, though this is pure speculation, when using a cervical ring like the NuvaRing). Again, add long sit times, an injury perhaps, and we can begin to see how the risk for blood clots in the female athlete using hormonal contraception can be much higher than for her teammates who do not use hormonal contraceptives.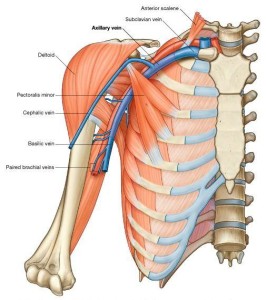 It is believed that the repetitive trauma that these sports require imposes strain on the subclavian vein leading to microtrauma of the endothelium and activation of the coagulation cascade. This alone is a risk factor for developing a blood clot, but when we add a few more variables, an intense competition, dehydration, a long flight home with upper body immobility and perhaps compression (sleeping on one’s arm), and enter these variables into an system primed for coagulation by hormonal birth control, the risk for dangerous blood clots increases significantly.
It is believed that the repetitive trauma that these sports require imposes strain on the subclavian vein leading to microtrauma of the endothelium and activation of the coagulation cascade. This alone is a risk factor for developing a blood clot, but when we add a few more variables, an intense competition, dehydration, a long flight home with upper body immobility and perhaps compression (sleeping on one’s arm), and enter these variables into an system primed for coagulation by hormonal birth control, the risk for dangerous blood clots increases significantly.