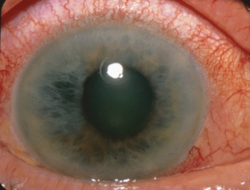
Two days ago, I helped my twelve year old daughter pack for two weeks of overnight camp. We followed the suggested packing list that the camp provided, and when we got near the bottom of the list I realized there was one important thing that was not there that she needed—her medication and supplements. My daughter has had cyclic vomiting syndrome (CVS) since she was two years old, a disease that causes her to have frequent episodes of severe nausea, vomiting, and abdominal pain.
She has bravely managed this debilitating disease for 10 years. She has been going to camp for four years already, and every year she has had a vomiting episode at camp—one year while she was out on a canoe trip, and one year starting early in the morning on the day she was supposed to leave. When she was younger she used to have episodes like clockwork every two months, and as she got older, her episodes became less predictable, and more responsive to events in her life such as stress, fatigue, or even excitement. She would sometimes have three episodes within one month, and other times go for as long as three months without an episode. On average she would have one to two episodes per month.
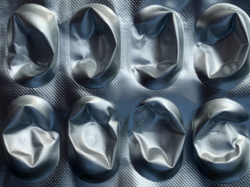
This year, for the first time, she has had only two episodes of vomiting in the last seven months. This dramatic change occurred after she started a new regimen of dietary supplements—L-carnitine and Coenzyme Q10. We decided to try using these supplements after learning about research that suggests that CVS may be caused partly or completely by mitochondrial dysfunction. More information about the connection between CVS and mitochondrial dysfunction can be found here. L-carnitine and Coenzyme Q10 assist the mitochondria with energy production and thus, help compensate for mitochondrial dysfunction and potentially improve symptoms in CVS patients. These supplements may also help improve symptoms in other disorders linked to mitochondrial dysfunction such as migraine, irritable bowel syndrome, fibromyalgia, and medication adverse reactions.
Results from small clinical studies on the use of these supplements for cyclic vomiting syndrome have been very promising. A retrospective chart review study found that using these two supplements, along with a dietary protocol of fasting avoidance (having three meals and three snacks per day), was able to decrease the occurrence of, or completely resolve, the CVS episodes in many patients. The supplements were also shown to be safe and well tolerated, with few side effects.
My daughter noticed an immediate improvement in her symptoms. She had almost daily morning nausea even when not having a vomiting episode, and this disappeared almost right away. She started asking for breakfast, when previously I’d always had to try to convince her to eat at least half a piece of toast. She now will often eat either three eggs and two pieces of toast, or a big plate of dinner leftovers for breakfast. She also has a better appetite throughout the day. I don’t think I ever heard her say the words “I’m hungry” until this past year, when she was 12 years old. Previously quite underweight, in the past 7 months she has literally gained as much weight as she gained in the previous 7 years.
The first 2 months on the supplements she had no vomiting episodes. Then she ran out of her supplements while my husband and I were away, and within 2 days she was having a vomiting episode. Then over the last 5 months she has had one more episode, after a period of extreme stress. This represents a huge decrease in episode frequency for her. When we got to packing her medications and supplements for camp, I packed her supplements with careful instructions for the doctor as to the dosage, and the fact that she has to take them every day to prevent episodes, as we saw earlier this year what happens when she stops them even briefly. I then started looking around the house for her Zofran pills (a strong prescription anti-emetic), which was what we would usually use to try to stop her vomiting when she was having an episode. I have always sent them to camp with the instructions that they are to be used if she starts vomiting. I couldn’t find the Zofran anywhere—it had been so long since we had needed it. I called the pharmacy, but they didn’t have any in stock. I found one emergency pill stashed in my purse and I packed that, but I have a feeling that this could be her first year enjoying camp with no interruptions due to illness.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Postscript: This article was published originally in July of 2014. We are happy to report that after years of suffering from CVS, Philippa’s daughter remains largely episode free with relapses only when she misses her supplements or changes her routine. For more on cyclic vomiting syndrome search our archive.